A tumor board, also referred to as a cancer treatment board, is a vital treatment planning process where a multidisciplinary team of cancer doctors and healthcare specialists come together regularly to evaluate and discuss complex cancer cases. The collective aim is to determine each patient’s most effective treatment plan.
These meetings convene medical experts from diverse areas of healthcare, including medical oncologists, radiation oncologists, surgeons, pathologists, radiologists, genetics experts, nurse specialists, physical therapists, social workers, and other healthcare professionals. Patients receive personalized treatment strategies through this collaborative multidisciplinary approach, ensuring improved clinical outcomes and patient satisfaction.
This article discusses the current state of tumor boards and common challenges to virtual cancer panels.
Why tumor board reviews are an essential part of improved clinical outcomes?
Tumor boards provide a comprehensive approach to cancer care by streamlining the clinical decision-making processes. A recent American Society of Clinical Oncology (ASCO) survey revealed that 96% of respondents1 noted that cancer treatment board meetings were beneficial to the cancer patient. They also provide educational value to oncologists and the rest of the care team.
In-person processes are time-consuming for a doctor and other health care providers. Hence the need for virtual meetings. Additionally, the COVID pandemic made online diagnosis and treatment the only logical way to bring doctors and other health professionals together to share knowledge, cutting-edge treatments, and discuss treatment options.
Why virtual tumor board reviews are the future of cancer diagnosis for health care providers?
A clinical study2 by researchers from Rutgers Cancer Institute of New Jersey discovered that physician attendance at tumor board reviews increased by 46% when an in-person multidisciplinary tumor board was made virtual.
Also, the research discovered that patient case presentations were faster, with a 20% increase compared to in-person tumor boards. Despite these benefits, there are still some sticking points or challenges to make virtual meetings efficient and productive for everyone involved.

Challenges of virtual tumor board meetings
The Covid-19 pandemic accelerated the transition of tumor board reviews online. Despite the efficiency and ease of conducting them virtually, there are multiple challenges3, particularly when it comes to using technology. Here are a few common obstacles to online tumor board review.
Synchronous schedules
Most virtual tumor board panels only accept oncologists based in a specific region and timezone. The organizers of these treatment meetings want members who can participate at a particular time. Other factors can deter oncologists and other healthcare professionals from partaking in scheduled tumor board meetings.
For instance, an oncologist who runs a busy clinic or works at a cancer center may either be too exhausted or unavailable for an appointment. This underscores the need for a flexible platform that allows multidisciplinary teams to participate at any time seamlessly.
Technical issues
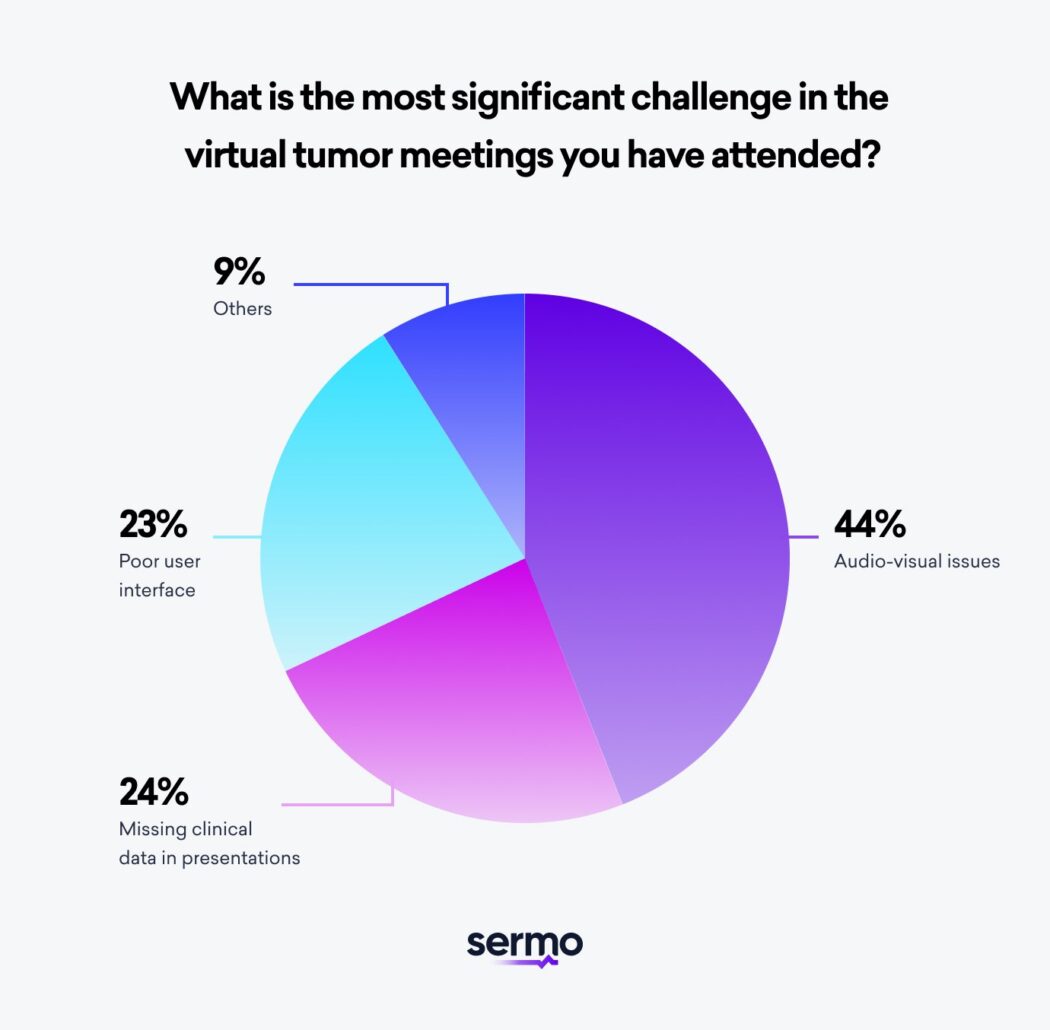
Virtual tumor board members may experience technical issues that occasionally interfere with their access to the online platform and active participation. For example, unstable internet connection and incompatible laptop or mobile devices may hinder easy access to the platform. A 2022 Sermo survey of physician specialists4 in our community revealed that audiovisual challenges were the most common technical issues in virtual tumor board diagnosis and treatment meetings.
Also, if the virtual tumor board platform is not user-friendly, some members may require extra time to learn how to use the tool. These pain points can create frustration for some participants who may feel they are spending too much time on an administrative task that keeps them from practicing medicine and helping patients.
Unorganized meetings and case discussions
Some platforms for hosting virtual tumor board meetings do not have the features required to sort and extract topics, cancer diagnosis or clinical trials discussed by different specialties. Consequently, tumor board members may experience challenges searching for cases, treatment care plans or topics relevant to the individual patient and cancer type.
In contrast, if the virtual platform has the ability to organize past tumor board meeting posts or discussions, new or current board members can quickly select cases they have sufficient knowledge and expertise to contribute fresh perspectives. This improves the likelihood that pathologists, surgeons, and other medical professionals will share their cancer expertise.

How to overcome challenges
The type of platform you host your virtual tumor board meetings on is essential to overcoming most of the highlighted challenges. Here are specific qualities of an ideal platform for virtual tumor board review.
Asynchronous meetings to discuss cancer cases
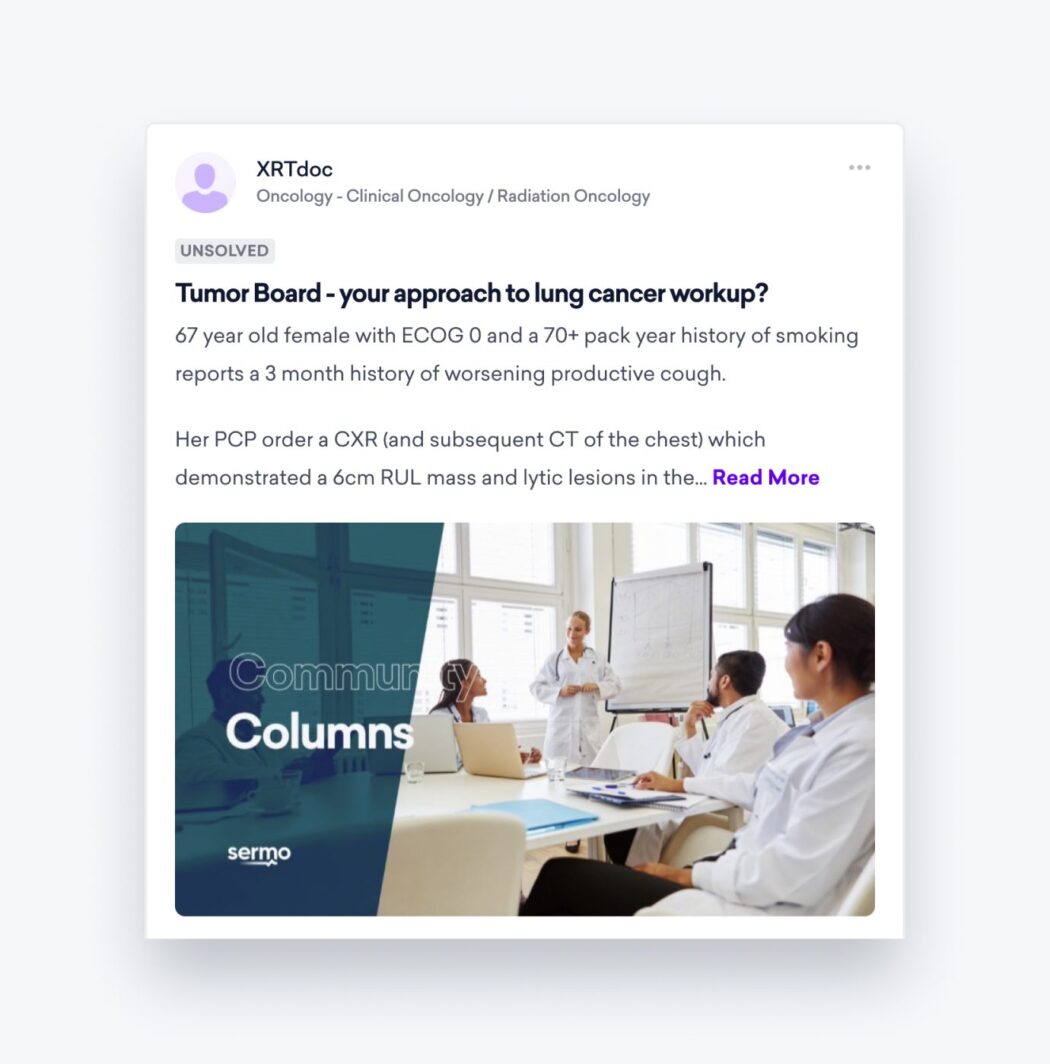
A platform that supports asynchronous meetings allow oncologists and other specialists to participate in case discussions and engage in these meetings on their own time. This makes tumor board meetings flexible to accommodate members who may not be available for meetings that conflict with other aspects of clinical practice. The Sermo virtual tumor board is a leading solution that fosters input from qualified oncologists regardless of location.
Global collaboration to guarantee fresh perspectives in line with cutting edge cancer care
Empowering the participation of licensed oncologists and physician specialists anywhere in the world promotes the quality exchange of ideas and continuous learning process in virtual tumor board meetings. Consider joining or hosting your meeting on a platform that allows the global contribution of licensed specialists.
Customized settings to securely review diagnoses and determine the best medical treatment options
Generally, most tumor board platforms are not user-friendly. “The technology for medical professionals has not been physician-user-friendly, it is just IT-user-friendly,” a specialist in the Sermo community reported in our survey.
Modern virtual tumor board platform should have the capacity that allows its members to sort past meetings based on specific preferences such as case topics, specialties, dates, etc. This will enable participants to find their preferences or specific details easily and quickly.
Consistent and frequent clinical case discussions
Keeping up to date with new medical information is crucial for success. Unfortunately, according to our recent Sermo specialist survey, only 58% of respondents reported consistent updates in their virtual tumor boards. These updates are vital for keeping members active and well-informed, ensuring they have access to the latest cancer treatment approaches that other oncologists share and reference during case discussions.
For consistent information updates on a virtual board, the organizer of the meeting may choose to delegate this task or leverage a community-based approach where doctors within one’s network can share the relevant research they are aware of.
Do you need tips to improve your meetings?
A virtual tumor board review is an efficient way for multidisciplinary experts in cancer care to share their knowledge and proffer comprehensive treatment plans for cancer cases. The features of the platform play a critical role in overcoming some challenges of conducting meetings remotely.
You will get tips and recommendations from other oncologists on how to efficiently conduct virtual tumor board meetings in your center by learning from the network of oncologists in a physician community like Sermo.
Sermo grants members access to a virtual tumor board and an online community comprising oncologists and over 1 million doctors across 96+ specialties. Our platform enables seamless collaboration and knowledge-sharing among medical experts.
Plus, you will be invited to exclusive earning opportunities and physician-only resources. It’s a triple win for you, your patients, and the larger medical field.
Common cancer patient and doctor questions about care team meetings:
What is a tumor board?
A tumor board is a multidisciplinary team of medical and radiation oncologists, surgical oncologists, pathologists, chemotherapy physicians, nurse specialists, therapists, social workers, genetics experts, and other medical professionals.
They work together to share expertise, review the diagnosis, and determine the best treatment options based on different cancer types. By involving different specialties, the tumor board meets with the mission of providing the best patient outcome possible.
Cancer center, clinical practice, and NCCN® guidelines for tumor boards
It’s paramount that cancer boards adhere to government, healthcare, and clinical practice guidelines. The NCCN Clinical Practice Guidelines in Oncology provide evidence-based recommendations. They are continuously updated to reflect evolving data as new cancer research and clinical trials are published.
Their purpose is to help oncologists and other oncology health care professionals make the major clinical decisions encountered in managing cancer patients by providing ready access to the highest quality information available based on the evaluation of expert clinicians from NCCN Member Institutions.
The National Comprehensive Cancer Network® Guidelines provide recommendations for appropriate cancer care for about 95% of patients; however, individual patient circumstances must be considered when applying these recommendations.
In all cases, clinicians need to be aware of the current clinical status of the patient. This includes general health, cancer type specifics, personal treatment plan preferences, plus current and former cancer therapies. Once the patient’s condition is assessed, a comprehensive approach, combining multidisciplinary perspectives and adhering to the highest standards of care, can be applied to individual patient cancer cases.
What is an example of a tumor board process?
Imagine a patient with a stage 2 lung cancer diagnosis. There are many factors involved with delivering a safe and effective cancer management treatment plan. How soon should the patient care plan begin? Are you absolutely positive the diagnosis was accurate? How will the patient manage chemotherapy, surgery, or other life-altering procedures?
In the tumor board meeting, the patient’s medical history, symptoms, imaging, possible health outcomes, and biopsy results are presented. The pathologist provides information on the type of cancer and relevant genetic testing. The radiologist presents imaging to assess the lung cancer tumor stage and spread. The multidisciplinary team discusses treatment options, considering the patient’s health, tumor characteristics, and biomarkers.
The treatment plan may involve surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, or palliative care. After communication with the patient, the chosen treatment plan is implemented, with regular reviews and updates by the tumor board. This ensures personalized and effective patient management care to maximize cancer survival rates.
Why are cancer boards multidisciplinary?
It’s not realistic that one doctor can accurately answer every question associated with the individual care plan. This is why the tumor board meets. To bring in expertise across different areas of medicine to review the diagnosis, discuss treatment options, and share fresh perspectives from promising clinical trials. Together, multidisciplinary teams are more successful than a solo doctor or even a group of medical oncologists.
How often are tumor boards used?
Although the frequency may vary, tumor boards usually have a regular schedule, either weekly or monthly, to review challenging or uncommon cancer cases. The participants are usually from the same hospital, but some tumor boards may also include doctor particiaption from affiliated hospitals.
Difference between Oncology second opinions and tumor boards?
Obtaining an oncology second opinion means getting an expert review of an individual’s diagnosis and treatment plan from a hospital that specializes in their unique cancer condition.
Mayo Clinic found that 88% of second opinions lead to a refined or distinctly different cancer diagnosis than the original diagnosis. Out of the 286 patient diagnoses reviewed in the study, a mere 12% of specialists consented with the initial diagnosis.
Access to tumor boards varies, particularly if your hospital lacks cancer specialty expertise or a dedicated tumor board, or if your case isn’t chosen for review. In such instances, it is advisable for patients to consider seeking a second opinion from surgical Oncologists or an Oncology specialist at a cancer specialty hospital.
Doctors who want to participate in virtual tumor boards or conduct their own can join Sermo for free today.