How much regulation is too much when it comes to women’s reproductive health rights? This is a pressing question for physicians who are navigating the ethical, safety, and accessibility challenges of their profession.
Physicians themselves are divided. In a recent Sermo survey, 53% of doctors supported no IVF regulation, while only 11% advocated for full regulation. For abortion services, opinions were similarly split, with 48% opposing regulation and 15% supporting it.1 What accounts for these differences and how do they impact patient care?
This article examines how physicians in the Sermo community perceive government involvement in fertility law and reproductive healthcare.
Understanding government regulation in IVF treatments
IVF treatments, essential for many infertile couples, are regulated inconsistently across states and countries. This inconsistency creates disparities in access and raises ethical concerns. For example, a recent Alabama ruling equated embryos outside the uterus to children,2 sparking fears about caps on embryo creation, bans on freezing backup embryos, and increased treatment costs.
One Sermo member for Family Medicine captured these concerns: “The new law in Alabama that equates embryos with children raises concerns about the future of IVF. There are fears of restrictions on the creation and use of embryos, negatively impacting accessibility. An open dialogue is necessary to establish a clear legal and ethical framework that protects the rights of all parties involved.3”
Sermo’s poll highlights the varied perspectives among physicians regarding government IVF legislation and regulation:
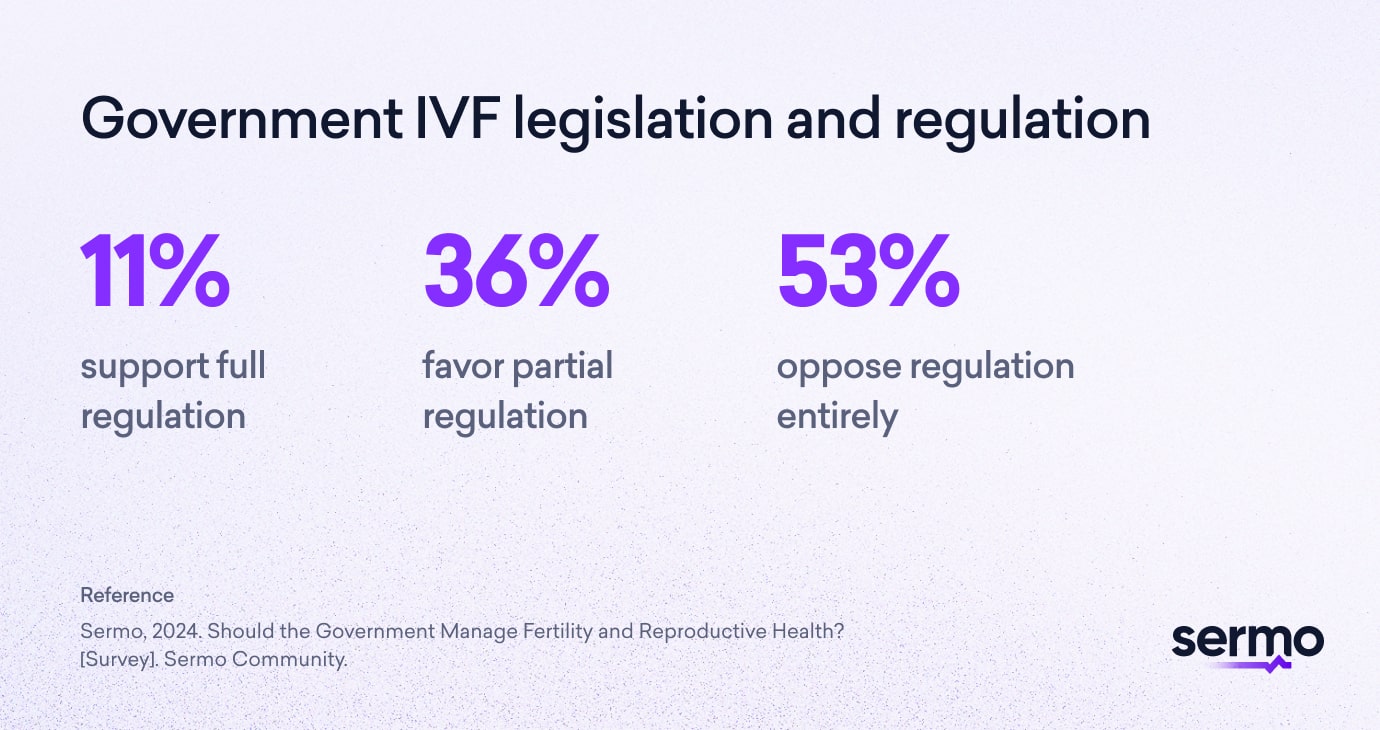
These results demonstrate a clear divide among healthcare professionals (HCPs), with a majority advocating for minimal or no government interference.
Physicians have expressed concerns that excessive government intervention could harm patients by causing:
- Reduced patient choice: “Reproductive decisions should not be controlled by government edict,4” stated a family medicine practitioner. “Having a child is a large enough decision without fear of government reprisal or being able to travel to have a procedure such as IVF done safely.”
- Increased costs and inefficiency: Caps on the number of embryos or bans on freezing could make IVF treatments less effective and prohibitively expensive.
- Unequal access: Varied regulations across states could create disparities, limiting options for patients based on geography. On the other hand, the potentially incoming Trump IVF policy could give greater access by funding treatment but with greater regulation.5
While physicians diverge on the degree of regulation, many agree on a shared benchmark: regulations should prioritize safety without compromising autonomy.
“Government involvement should only apply to the safety of facilities and not in healthcare decision-making,4” emphasized a physiatrist.
By maintaining this delicate balance of prioritizing safety within regulation, physicians believe it’s possible to support access, equity and patient-centered care in reproductive health services.
Innovations may force more regulation

While many Sermo members advocate for minimal government involvement focused primarily on safety, the rapid pace of technological innovation in IVF could necessitate expanded regulatory frameworks.
Innovations like the BELA AI system, which enhances IVF by accurately assessing embryo quality and eliminating bias, are reshaping reproductive healthcare. As Dr. Nikica Zaninovic noted, “BELA and AI models like it could expand the availability of IVF to areas without high-end technology, improving equity worldwide.6”
However, such advancements bring new regulatory challenges. IVF law frameworks may need to be expanded to ensure ethical standards and consistency concerning:
- Data security
- Equitable use
- Standardization across diverse regions6
Policymakers face the delicate task of fostering innovation while safeguarding equity and trust, emphasizing the importance of collaboration between physicians, technologists and regulators to maintain patient-centered care.
Examining abortion legislation: where do physicians stand?
Abortion legislation in the United States remains one of the most polarizing issues in healthcare, affecting not only patients but also the physicians tasked with providing care.
State-level restrictions, like those enacted in Alabama, expose the intricate tension between medical ethics and politically driven policies. “In the USA, issues about treating people for reproductive reasons or with hormonal medications depend upon the politics of the state,7” noted an internal medicine practitioner. This entanglement of politics and healthcare raises critical concerns about how regulations influence patient outcomes and physician practices.
Sermo survey data reveal the spectrum of doctors opinions on abortion regulation:
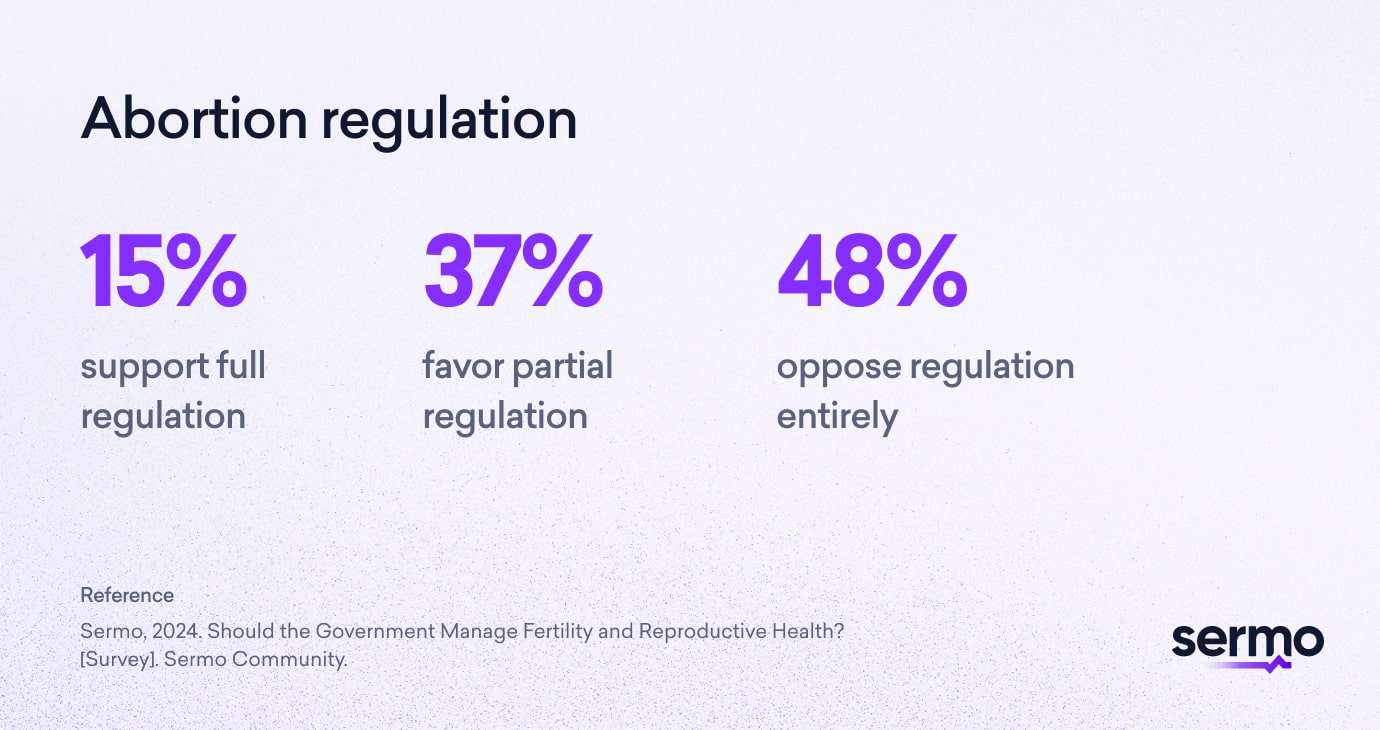
This split reflects a fundamental tension between doctors and abortion: while some physicians view abortion laws in the USA as a tool for maintaining ethical oversight, others see it as a barrier that undermines patient autonomy and access to care.
Why is abortion regulation so contentious?
Physicians often find themselves at the intersection of politics, ethics and medical practice, grappling with laws that claim to protect patients but frequently introduce unintended consequences. The key concerns surrounding restrictive abortion regulations include the following:
- Compromised Safety: Laws restricting abortion services often push procedures underground, leading to unsafe practices and increased risks for patients.
- Limited Access: Rural and underserved areas bear the brunt of restrictive policies, leaving vulnerable populations with few, if any, options for care.
- Politicization of Healthcare: When laws are driven by ideological agendas, they erode trust in the doctor-patient relationship and hinder physicians’ ability to deliver unbiased, patient-focused care.1
“I’m sickened by the notion that physicians were/are swayed by politics and/or religion in such a way that patient care was/is impacted,” said a physiatrist. “Patients need to be informed of such beliefs ahead of time.7”
Regulation can make for reduced access
The ripple effects of restrictive abortion laws extend beyond individual patients, influencing the healthcare system as a whole. Physicians report being driven away from regions with strict regulations, exacerbating existing workforce shortages in underserved areas.
“The growing physician shortages highlight the impact of political decisions on healthcare,7” explained a general practitioner in Argentina. “The exodus of doctors from regions with restrictive policies, like abortion bans, shows how these pressures can influence where we choose to practice, ultimately affecting patient care.”
This phenomenon leaves communities, particularly in rural or conservative areas, without sufficient medical support, compounding inequities in healthcare access. A family medicine physician in Cuba highlighted this inequity: “Due to political problems, there is a shortage of resources and medicines, making it very difficult to work. Many leave to improve their finances because the payment is very little7.”
The shared view amongst these physicians is that reproductive legislation should prioritize healthcare accessibility and workforce retention.
Ethical considerations: Autonomy vs. Regulation

For many physicians, abortion care is an ethical minefield, particularly when restrictive laws conflict with patient autonomy. Emergency abortion cases highlight this tension, where doctors must balance legal mandates against their ethical obligation to save lives and prioritize patient well-being.
“Medicine and healthcare should be guided and governed by laws that protect the rights of the patient and medical professional alike,7” emphasized a pathologist. Yet these laws often heighten moral dilemmas, particularly regarding the rights of embryos, which further complicate decision-making.
As one internal medicine physician reflected, “The creation of embryos lend themselves to the possibility of destruction, raising ethical concerns.4”
Restrictive abortion legislation in the US also has a profound impact on the doctor-patient relationship. Trust and confidentiality, essential pillars of effective care, are threatened by policies that prioritize ideology over patient welfare.
“Politics and politicians seldom get things right,” remarked a general surgeon in the U.K., “and the more they tinker with things (especially those that were working before), the more they’ll be messed up.7”
Despite differing opinions on abortion regulation, there is a shared consensus among physicians: policies must prioritize patient safety and autonomy while avoiding the politicization of care.
Problems associated with government involvement in reproductive healthcare
The impact of government regulations on reproductive healthcare reshapes the experiences of both physicians and patients. While regulation can provide safeguards, many HCPs view excessive government involvement as a threat to autonomy and the quality of care they deliver.
Sermo’s data underscores these concerns. Physicians identified several key risks associated with government overreach in reproductive healthcare:
- 17% cited infringement on personal freedoms
- 4% worried about decreased safety and ethical standards
- 7% flagged limited availability of services
- 2% noted risks to patient confidentiality
- 21% pointed to the politicization of healthcare decisions
- Most strikingly, 48% highlighted all of these risks combined1
One internal medicine practitioner voiced a common sentiment: “In our patient-centered care models, patients should be allowed to make decisions on their embryos.3”
For many doctors, managing patients requiring abortion or fertility services has become a daunting task, with 69% of surveyed physicians expressing concerns.1 The fear isn’t abstract; it directly affects their ability to provide ethical, patient-focused care.
To counter these challenges, physicians advocate for policies that prioritize patient safety without compromising their autonomy or the decision of the doctor. “A politician knows nothing about medicine, unless that politician is a doctor and has experienced the everyday situations that are experienced in a health center or in a higher level establishment,7” stated a GP.
Your takeaway
As Sermo survey data shows, government involvement in reproductive healthcare reveals deep divides among physicians. While some view regulation as necessary for safety and ethical oversight, others fear it undermines autonomy and access.
Key challenges include restrictive laws driving inequities, politicizing care and eroding trust in the doctor-patient relationship, while innovations like AI in IVF add complexity, emphasizing the need for thoughtful, balanced policies.
Physicians advocate for frameworks prioritizing safety and equity without overstepping into ideological agendas, ensuring reproductive healthcare remains compassionate and patient-centered.
Join the conversation shaping the future of reproductive healthcare
Join Sermo today and be part of the global physician community shaping the future of healthcare. Share your insights on reproductive rights and other critical issues, connect with peers, and help influence balanced, patient-centered policies.
Footnotes
- Sermo, 2024. Should the Government Manage Fertility and Reproductive Health?
- BBC Future, 2024. What is an embryo? Global medical definition of personhood IVF ruling.
- Sermo, 2024. Comment on Poll: Should the Government Manage Fertility and Reproductive Health?
- Sermo, 2024. Comment on Poll: Day 2—Infertility Awareness Promo.
- BBC News, 2024. Trump says insurance or government should pay for IVF.
- Weill Cornell Medicine, 2024. A fully automated AI-based system for assessing IVF embryo quality.
- Sermo, 2023. 64% of doctors say politics affects their medical practice.