Double-booked schedules, mounting administrative loads and dwindling time with patients have become the new normal for many physicians. These pressures reflect a larger issue: the U.S. could see a physician deficit of up to 86,000 by 2036. The issue also persists on a global level; the World Health Organization (WHO) projected a shortfall of 11 million health workers by 2030.
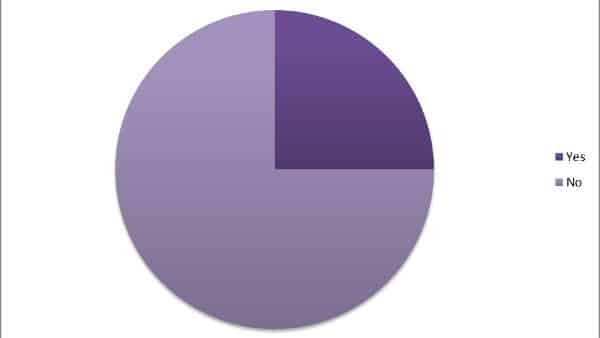
A Sermo survey found that 56% of participants currently work on a short-staffed team, and 27% have in the past. Further insights from the Sermo community illustrate how the physician shortage is affecting doctors, and which strategies could mitigate the crisis.
How the physician shortage is affecting the daily life of doctors
Sermo members are already feeling the effects. In a poll about the effects of working on a short-staffed team, 28% said they spend more time working outside of business hours, 26% have noticed increased stress/burnout, 22% fear making mistakes, and 18% said they aren’t able to see as many patients.The doctor deficit has significant implications for healthcare in the U.S. Some of the most affected areas include:
- Primary care physician shortage: A report from the Association of American Medical Colleges (AAMC) predicted a shortage of 17,800 to 48,000 primary care physicians by 2034, with rural areas being most vulnerable. When fewer PCPs are available, patients experience longer wait times and may skip routine care altogether, leading to higher rates of preventable illness and hospitalizations.
- Emergency medicine: In 2023, there were 554 unfilled residency positions in this field. As emergency departments face staffing gaps, physicians may have to manage more patients simultaneously, increasing the risk of errors and delayed care in critical situations. Overcrowding can also strain inpatient teams downstream, as patients remain in the ED longer waiting for admission.
- Medical specialties: Medical specialties such as cardiology, oncology and pulmonology are projected to have a shortage of 3,800 to 13,400 physicians by 2034, according to the AAMC report. Shortages in these areas mean patients may wait months for appointments, potentially delaying diagnosis or treatment for serious diseases such as cancer or heart failure.
In discussions about staffing issues, members bring up the effects of burnout. “It’s a vicious circle – burnt out staff leads to increased absences which further increases the pressure,” laments a general practitioner. A general surgeon writes that staffing issues have “a huge effect” on burnout, and that as a result, “physicians are prone to mistakes, can suffer from mental issues, can fall ill et cetera.”
Often, employers lack the funds required to address staffing issues, according to another general surgeon and Sermo member. “Short staffing seems to be a worldwide issue and yet vacant jobs are often hard to find as there is no active recruitment due to financial constraints,” they write.
The emotional toll of the physician shortage on doctors
Short staffing can affect how physicians view their careers, their satisfaction with their positions and their plans for the future. “Short staffing is a serious issue, and its connection to burnout is both well-documented and deeply concerning,” according to a GP on Sermo.
The emotional toll of physician burnout goes beyond exhaustion. It includes moral distress, professional dissatisfaction and a sense that the conditions necessary for quality care are eroding.
A Sermo poll investigated how staffing changes have affected members’ thoughts about their current position. While 36% said it hasn’t changed their opinion, 23% are considering reducing their hours, 24% are considering leaving for another position, and 13% are contemplating retirement.
A GP described compounding challenges: “I work for a low income area, the area isn’t very desirable so we have a hard time trying to recruit people,” they share. “When we do, I feel that we don’t find the most qualified people who put out patients’ best interest first.” Similarly, a radiation oncologist writes that the “cycle of overwork and attrition only worsens the situation.”
One emergency medicine physician believes that external pressures exacerbate burnout from staffing issues. “I feel that the way the public views us physicians especially after the pandemic is also a large part for burnout,” they explain. “As an ED physician there are more expectations and more opinions. It is as if they do not trust us anymore and come with more demands.”
Strategies for addressing the physician shortage
Strategies to improve immediate working conditions as well as long-term retention can help address the ongoing physician shortage. In a poll, Sermo members shared the approaches their organizations are currently using, including actively recruiting (32%), offering recruitment bonuses (12%) or offering hiring bonuses (8%).
Actively recruiting
Traditional recruitment efforts remain the most common strategy. Organizations can expand their search beyond local markets, attending career fairs and working with placement agencies to identify qualified candidates. Even smaller practices can benefit from creative outreach, such as offering flexible schedules, telemedicine options or mentorship opportunities to attract early-career physicians. This can have positive knock-on effects, according to an internist on Sermo. “I believe better staffing and implementing more people during each shift would maximize patient experience so things don’t go unnoticed,” they argue.
However, recruitment alone doesn’t address the underlying issues that make positions difficult to fill or retain.
Offering recruitment bonuses
Some organizations are leveraging their existing workforce to expand recruitment reach. By incentivizing current physicians to refer qualified candidates, organizations tap into professional networks that might not respond to traditional job postings. This approach can be particularly effective in specialties where personal recommendations carry significant weight.
Offering day one bonuses
Financial incentives like signing bonuses can make positions more attractive, especially in competitive markets or underserved areas. While money alone won’t solve the shortage, it can help offset the challenges of relocating or taking on positions in less desirable locations.
Improving workplace conditions
Flexible scheduling, remote work options for certain administrative tasks, and part-time positions can appeal to prospective hires. These accommodations recognize that physicians have lives outside of work and that flexibility can be a powerful retention tool. A cardiologist on Sermo advocates for “investing in staff wellness programs to help reduce burnout and improve retention.”
An OBGYN shared a practical approach: “I think that if a hospital is short on staff they should distribute professionals where they are most needed. As professionals, we should be able to prioritize which patients require immediate care no matter what and which can be deferred to a moment in which colleagues can help out.”
While physicians can’t singlehandedly solve the shortage crisis, they can take steps to protect their boundaries in hopes of avoiding burnout due to staffing issues. A family medicine doctor on Sermo made a case for physicians communicating their needs. “I think we need to try to manage stress better, if possible, work fewer hours, and continue to demand our rights,” they advise. “As a suggestion, we could talk about the physicians who have changed positions and even specialties throughout our working lives in search of a better quality of life and care.”

The physician’s role in advocating for change in healthcare
While solving the physician shortage will require a broad shift within healthcare systems, physicians can help play a role in shaping solutions.
Sermo polling data shows how physicians view their role in advocating for better staffing practices. 41% believe in clearly communicating their needs. Physicians who document staffing challenges, share patient care concerns with administrators, and provide concrete examples of how shortages affect outcomes can drive institutional change.
17% of respondents favor participating in administrative roles. This gives physicians direct influence over staffing decisions and resource allocation. While not every doctor wants to take on these responsibilities, those who do can bridge the gap between clinical needs and organizational constraints.
10% support unionization. These approaches can amplify individual voices and create negotiating power around staffing levels and working conditions.
Government-level advocacy, while pursued by a smaller percentage (6%), can have a powerful effect. Policies around medical education funding, visa programs for international medical graduates and reimbursement rates can all affect the physician supply pipeline.
What the physician shortage means for doctors
The physician shortage is fundamentally changing how doctors practice medicine. It affects workload, emotional well-being, career satisfaction and the ability to provide quality patient care.
Feedback from Sermo members shows that this shortage means more than just longer hours and busier schedules. It represents a threat to the core values of the profession. When doctors can’t spend adequate time with patients, when they’re too exhausted to perform at their best, when they’re considering early retirement because the conditions have become unsustainable—the entire healthcare system suffers.
Physicians can speak up about the conditions, sharing experiences with institutional leaders, participating in policy discussions and advocating for change. Beyond voicing concerns informally, they have a professional responsibility to share their experiences with institutional and leaders—whether through hospital committees, medical associations or advocacy groups—to help shape policies.
The physician shortage has widespread implications that are very real to many practitioners, but shared experiences and collaboration can inspire solutions. Join the Sermo community to engage with fellow healthcare professionals, share your insights and participate in ongoing discussions about finding real-world solutions to this crisis.