Ever wondered how much doctors make?
Spoiler: It’s more than most people think, but the story doesn’t end there! In some places, doctor’s salaries have actually stagnated or fallen in relative buying power over the past decade.
Understanding physician pay provides valuable insights into the healthcare industry and influences everything from career choices to healthcare costs.
In Sermo’s physician compensation report, we reveal critical trends, pay disparities, and salary satisfaction levels shaping the industry.
Overview of physician compensation
This physician compensation reports paint a comprehensive picture of earnings in the medical profession. On average, physicians in the United States earn $352,000 annually, marking a slight increase from the previous year.
Average physician income in Europe varies between €52,000 – €280,000 per year, depending on position and experience. The countries with the strongest pay relative to cost of living in the EU are Germany (€100,000 – €280,000), Netherlands (€150,000), Denmark (€150,000), and Ireland (€120,000). Internationally, Japan also ranks high in terms of pay.
These above-average salaries reflect rising demand for healthcare services and the increased workload on physicians post-pandemic.
Sermo and other sites have found that about 62% of doctors feel they are fairly compensated, but this depends largely on the country surveyed.
General trends in physician pay
Steady increase with relative stagnation
The overall trend indicates an overall increase in physician compensation, with significant variations across different specialties and regions. This rise is partly due to growing populations, the growing complexity of medical procedures, and the increased demand for specialized care.
It is important to note that relative to purchasing power or compared to the average salary in the country, doctor’s salaries have actually decreased in many countries (and in some American states).
For general practitioners, the ratio of net income to the national average wage falls within a range of 2 to 3.2 across most countries. Physicians in Japan had the highest net pretax income at 7.3 times the average wage, compared to 4.4 in Germany and 3.9 in the United States.
Over the years, physicians’ net income has not risen as fast as national average wages, especially for GPs. This will be a critical trend to monitor in the coming years as it’s well-noted that dissatisfaction in pay often leads to burnout by physicians.
Specialized care demand
The increased complexity of medical procedures and heightened demand for specialized care have contributed to rising average physician pay.
For instance, the adoption of advanced technologies in cardiology and oncology, such as robotic surgery, personalized medical treatments, and artificial intelligence, has led to better patient outcomes and more technical procedures, which leads to higher income for specialists.
Technological adaptation
The widespread adoption of new computer technologies, such as telemedicine and electronic health records (EHR), has also influenced physician pay. These technologies have streamlined administrative work and improved patient care, allowing doctors to see more patients more often and enhancing their overall business productivity.
National average and specialty-specific compensation

National average
Physicians’ salaries vary based on specialty, experience, and location.
In the United States, primary care physicians earn an average of $260,000. Specialists take home about $368,000 annually. This disparity highlights the significant differences in compensation based on the type of medical practice.
This disparity unfortunately is also seen between male specialists and their female counterparts, with male specialists often earning more in the same specialty with the same level of experience. Read on to see how this impacts healthcare and what can be done.
Top-earning specialties
Certain medical specialties command higher salaries due to the specialized skills, advanced education, and legal risks involved.
The highest-earning specialties include:
- Neurosurgery: $750,000
- Orthopaedic Surgery: $450,000 – $650,000
- Plastic Surgery: $479,000
- Cardiology: $460,000
- Anesthesiology: $450,000
These specialties involve intricate procedures requiring years of additional training and significant expertise as well as expensive insurance coverage.
Additionally, vascular surgery and thoracic surgery are lucrative due to the high demand, low supply, and complex procedures involved.
Lower-earning specialties
On the other end of the spectrum, pediatricians and family medicine physicians are among the lower-paid specialties, earning $238,000 and $255,000 annually, respectively.
Despite the critical role these professionals play in providing primary care and early prevention, their income reflects lower reimbursement rates and the broader scope of services they provide. Rehabilitation and psychiatry are two more common specialties that rank in the lowest salaries.
Compensation by age and experience
Age and experience trends
The average physician’s income also varies significantly based on age and experience.
- Physicians under 35 earn $250,000
- 35 to 44 years old earn $350,000
- Over 45 years old earn $450,000
This trend underscores the importance of experience and age in determining physician compensation. Older and more experienced physicians generally earn higher salaries due to their advanced skills, workplace tenure, established reputation, and network.
Additionally, self-employed physicians often follow a similar wage increase over time as they gain experience and build their practice.
Career progression
As physicians gain more experience, they often receive more referrals, take on more complex cases, build a network, or even open their own practice. This allows physicians with more experience to leverage that experience and garnish higher wages. The data supports an upward trend in income relative to the career stage.
Compensation growth over time

Trends and projections
The average physician salaries have steadily increased over the past decade, with a modest 3% growth in total compensation from 2023 to 2024. This growth reflects the rising demand for healthcare services, the increased workload on physicians, and the growing complexity of medical procedures.
Additionally, the shift towards value-based care and the emphasis on preventive medicine have contributed to the steady increase in physician compensation.
Economic and policy factors
Economic conditions and healthcare policies, such as changes in Medicare reimbursement rates, significantly impact physician compensation.
For instance, recent Medicare reimbursement cuts have affected the real income of physicians, particularly those in primary care.
These changes highlight the need for continuous advocacy and policy reform to ensure fair compensation for physicians across all specialties.
Implications and impact
For physicians
Understanding compensation trends helps physicians make informed career decisions, negotiate better salaries, and plan for their financial futures.
By staying informed about industry trends, physicians can navigate the complexities of advocating for better working conditions and compensation structures.
For healthcare business owners
These trends are vital for effective practice management and recruitment. Competitive compensation packages are crucial for attracting and retaining top talent.
Additionally, understanding regional variations and specialty-specific demands can help healthcare organizations optimize their hiring strategies.
By offering attractive compensation and benefits, healthcare organizations can ensure high levels of job satisfaction and retention among their staff.
Factors influencing earnings
Level of risk
Surgeons generally earn more due to the high-risk nature of their work. Thoracic surgery and neurosurgery, which involve high-stakes operations, command higher salaries compared to less invasive surgical specialties.
Similarly, specialties like emergency medicine, which require rapid decision-making in high-pressure environments, also see higher compensation.
Demand for specific skills
Specialties in high demand and short supply, like emergency medicine and preventive medicine, often see higher compensation.
The growing emphasis on preventive care to reduce long-term healthcare costs has increased the value of specialties focusing on early diagnosis and management.
Furthermore, fields like pediatric cardiology and pediatric nephrology, which require specialized training and expertise, also command higher pay.
Nature of patient interactions
Specialties involving more frequent patient visits and longer-term care, such as psychiatry, tend to have lower compensation despite being crucial to overall healthcare. The continuous patient interaction required in these fields can limit the number of patients a physician can see, affecting overall earnings.
Additionally, administrative duties associated with mental health care can further reduce the time available for patient care, impacting physician pay. In many countries, mental health is sparsely covered by insurance, making it harder for patients to pay for treatment and more difficult for healthcare businesses to justify an increase in their doctor’s salary.
Geographic pay disparities
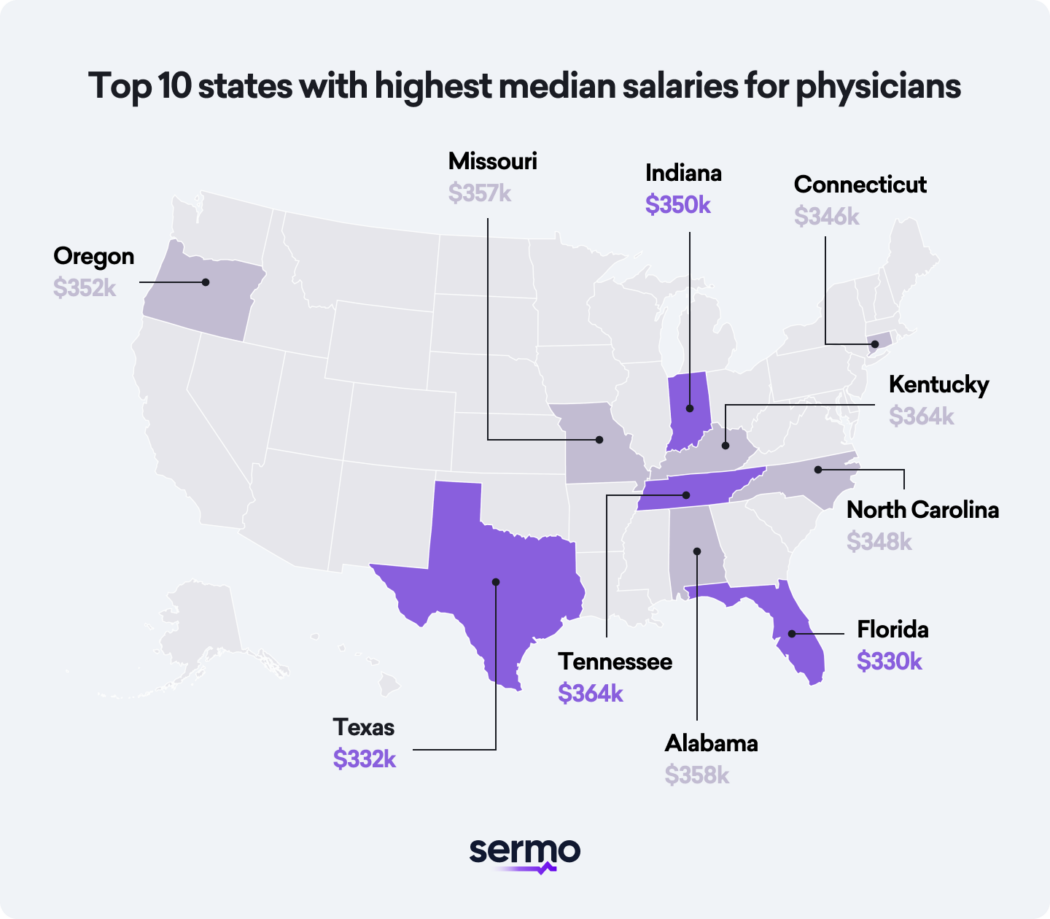

Metro vs. Rural areas
Physician compensation changes between metropolitan and rural areas. Most physicians in urban centers earn more than those in rural regions because of the higher cost of living and greater demand for specialized services.
For example, physicians in metropolitan areas like New York and San Francisco can earn up to 25% more than their counterparts in rural areas.
Regional variations
Significant pay differences exist between states, with physicians in states like California and New York earning considerably more than those in the Midwest.
For instance, the average annual compensation for physicians in California is $400,000, compared to $320,000 in Ohio.
These variations in average income are influenced by local healthcare demand, cost of living, and state-specific healthcare policies.
Regional variation in physician compensation
The average annual physician compensation in the United States varies significantly across regions.
Cost of living adjustments
When comparing salaries, it’s essential to consider the cost of living. A high salary in a metropolitan area might not stretch as far as a lower salary in a rural setting.
For example, a physician earning $350,000 in San Francisco may have a similar standard of living to one earning $250,000 in a rural area due to the higher cost of housing, transportation, and other expenses.
Gender pay disparities

Current statistics
Despite progress in gender equality, a significant pay gap persists for physicians.
The average physician income for both genders are:
- Male Physicians: $380,000
- Female Physicians: $307,000
This gap persists across nearly all specialties and practice settings.
Primary care physicians show a slightly narrower gap of 19% among physicians surveyed, but the disparity remains a pressing concern and an area for improvement.
Historical context of gender wage gap
While the gender pay gap has narrowed over the past decade, progress remains slow. Historically, female physicians have faced structural barriers and biases that have limited their earning potential compared to male physicians. Although more women are entering the medical field, the compensation disparity continues to be a top issue.
Possible causes
Several factors contribute to the gender pay gap, including differences in negotiation strategies, career interruptions for childbearing, disproportionate access to education, and part-time work preferences among women.
Additionally, women are underrepresented in higher-paying specialties and leadership positions, further exacerbating the income gap. Addressing these disparities is crucial for ensuring that all physicians are fairly compensated.
Impact on career satisfaction
Due to these disparities, women physicians often report lower job satisfaction, highlighting the need for more equitable income structures. This disparity can lead to increased stress, burnout, and even early career changes among female physicians.
Addressing these disparities is crucial for improving morale and retention among female doctors, especially as the need for quality healthcare continues to grow worldwide.
Racial and ethnic disparities
Compensation disparities
The report by NCBI also highlights notable trends in racial and ethnic compensation disparities. African American and Black physicians, for instance, earn significantly less than their white counterparts, with an average difference of $37,000.
These disparities are a pressing issue, emphasizing the need for greater diversity and inclusion in the healthcare workforce.
Efforts to address disparities
Healthcare organizations and professional associations are increasingly focusing on initiatives to address these disparities. Mentorship programs, diversity training, and policies aimed at promoting equal opportunities are some of the measures being implemented to bridge the gap.
Benefits and bonuses: parts of physician compensation

Incentive bonuses
Incentive bonuses, which can account for a significant portion of a physician’s income, are often tied to performance metrics such as patient outcomes, efficiency, and adherence to clinical guidelines.
For instance, physicians in plastic surgery and anesthesiology often receive substantial bonuses for achieving high patient satisfaction scores and successful procedural outcomes.
Fee-for-service (FFS) model
The fee-for-service (FFS) model is a traditional compensation approach that rewards physicians based on the average volume of services they provide.
While lucrative, this model has been criticized for potentially encouraging the overutilization of high-paying services and compromising the quality of care. Balancing FFS with value-based care models is essential for ensuring optimal patient outcomes.
Additional benefits
Healthcare organizations offer additional benefits such as flexible scheduling, telehealth, and workplace benefits to attract and retain top talent.
These benefits are crucial for maintaining job satisfaction and preventing burnout among physicians.
For example, offering locum tenens positions can provide doctors with the flexibility to balance work and personal life while still earning competitive salaries.
Career and compensation satisfaction
Overall satisfaction
In a recent Sermo survey, we found that 62% of physicians feel fairly compensated in the USA.
However, satisfaction levels vary by specialty and geographic location.
Specialty differences
Highest-paid specialties like dermatology and ophthalmology report higher satisfaction levels than primary care physicians, who often deal with lower compensation and bigger patient loads.
Additionally, specialists in fields like radiology and urology also report high satisfaction levels due to their higher incomes and better work-life balance.
Influence on career choices
Compensation plays a crucial role in career choices, with many medical students gravitating towards the highest-paying specialties. This trend impacts the availability of primary care physicians and other lower-paid specialists, which can affect overall patient care.
For instance, the shortage of primary care physicians has led to increased reliance on minute clinics and advanced practice providers to meet patient needs.
Gender and race pay gap
The gender and race pay gap also influences career satisfaction, with many minorities and female physicians reporting lower satisfaction levels as compared to their white male counterparts.
This disparity highlights the need for policies promoting equal pay and career advancement opportunities for all medicine. Addressing these issues is essential for improving job satisfaction and reversing the tidal wave of burnout in healthcare.
Other trends in physician compensation in 2024-2025

Innovative compensation models
Organizations are innovating their approaches to attract and retain top physician talent, prioritizing lifestyle enhancements like flexible scheduling, additional workplace perks, and remote work options.
These non-traditional benefits are becoming more popular as healthcare providers seek to improve the work-life balance for physicians.
Increased use of advanced practice providers (APPs)
Health systems increasingly turn to APPs as a strategic solution to address physician shortages.
APPs, such as nurse practitioners and physician assistants, bring advanced education and training, offering a multifaceted approach to patient care that aligns with the evolving needs of modern healthcare.
If you’re an advanced provider make sure to join the Sermo community built just for APPs.
Impact of regulatory compliance
Regulatory fines and legal restrictions can also impact how much physicians earn.
Healthcare providers spend nearly $39 billion annually on the administrative aspects of regulatory compliance across various domains like conditions of participation, billing, quality reporting, fraud and abuse laws.
The Stark Law prohibits physicians from being compensated based on the volume or value of their referrals to hospitals or other healthcare entities. This restricts tying physician pay directly to productivity metrics like relative value units (RVUs) that are linked to referrals.
Hospitals have faced major settlements for allegedly compensating physicians above fair market value (FMV) or in a manner that violates Stark Law, such as the $24 million settlement by a Montana hospital system accused of improper compensation agreements with over 50 physicians.
Another recent case involces Community Health Network Inc. CHN made a big mistake by paying doctors money to get them to send patients to CHN. This was against the rules.
A past employee reported this to the government. The government found CHN to be at fault and fined them $167 million. CHN had to agree to some new oversights to prevent it from happening again and make a plan to ensure they did the right thing.
Compliance with regulations is essential for maintaining financial stability and avoiding costly penalties.
Conclusion
The 2024-2025 Sermo Physician Compensation Report offers a glimpse into how much doctors are paid across countries, rage, gender, experience, and more. By understanding these trends and disparities, physicians and healthcare business owners can check to see how they compare to industry averages and what progress is left to be made.
Stay informed, advocate for fair compensation, and contribute to a more equitable and efficient healthcare system. As the healthcare landscape continues to evolve, staying updated on compensation trends will be crucial for ensuring that physicians are fairly rewarded for their dedication and expertise.
Sermo makes it easy to keep up to date in your specialty.
Physicians and APPs: Join today and claim your exclusive benefits.