Medical billing is a core operational aspect of every healthcare organization. And just like other administrative operations can be either outsourced or done in-house. Medical billing outsourcing has become increasingly popular and there are now a number of firms and agencies that take on this responsibility for healthcare organizations. However, some healthcare providers still prefer the good old method of handling billing themselves.
How do you know which is best for your practice? Read on to learn about how outsourced billing services work and whether it’s right for you.
What are outsourced medical billing services?
Revenue cycle management and payment collection are very important processes in every healthcare organization. These administrative functions including coding and billing can be very daunting and should not be taken lightly. Proper reimbursement of health organizations and physicians is highly dependent on efficient medical coding and billing and this is why healthcare organizations outsource their billing and coding.
To outsource medical billing means to contract a third party to handle and process all medical coding and billing tasks instead of completing it in-house. When health organizations outsource medical billing services to a third party, they entrust all the necessary information and data to the medical billing company and rely on their professional expertise to process claims and facilitate reimbursement.
By having a third party company take responsibility for medical billing, healthcare organizations can focus their energy more on delivering care to patients without worrying about getting paid. Medical billing and coding companies take care of:
- Claims filing
- Charge/coding review
- Claim submission
- Payment posting
- Fixing and reprocessing claim rejections
- Appeal denials
- Accounts receivable management
- Patient payments and statement call center
- Interacting and following up with insurance companies and other payers

Pros and cons of outsourcing medical billing
The medical billing procedure is both costly and time-consuming. Hence it remains a big question for many healthcare providers whether to or not to outsource medical billing services. Each healthcare organization has unique internal challenges, organizational structures, staffing levels, financial goals, and budgetary constraints that must be considered before deciding on outsourcing medical billing. Healthcare providers should consider the pros and cons of medical billing outsourcing before making a decision.
Here are some of the pros and cons to consider before choosing to outsource medical billing services.
Pros of outsourcing medical billing
1. Cost savings
You may have heard the saying “It costs money to get money”. This is exactly true for medical billing. Hiring and maintaining a highly skilled in-house billing department can be very expensive for a hospital. The overhead expenses to be incurred includes infrastructure installation costs, onboarding costs, training, salaries and benefits. Many healthcare organizations may struggle to keep up with the cost of managing an in-house billing department and so it makes sense to outsource this administrative chore.
Moreover, third-party billing companies enjoy economies of scale. Because they are a dedicated firm servicing a number of healthcare providers, the cost of their billing and coding operations is relatively lower compared to a healthcare provider. So they process a lot more billing claims at a cheaper rate.
2. More time to focus on patients
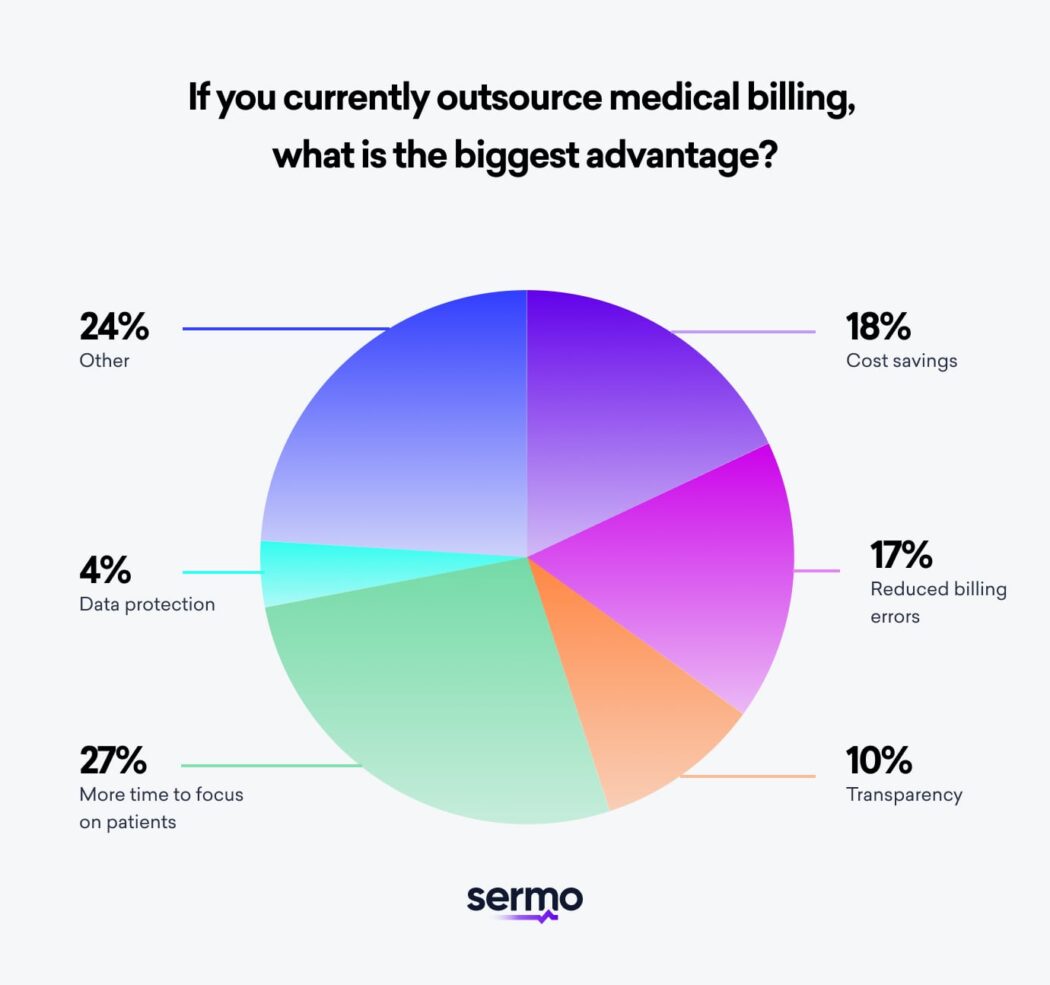
Billing is also a time-consuming task. It can be quite a cumbersome task involving going through records, punching numbers, reviewing codes, processing appeals and arguing with insurance companies. This takes time and resources away from other activities. In a Sermo poll, 26% of physicians indicated time saving as the biggest advantage of outsourcing medical billing.
By outsourcing medical billing, healthcare providers can focus more on delivering quality healthcare to patients. This is particularly beneficial for small practices who cannot afford to be overburdened with such administrative tasks on top of their main responsibilities.
3. Reduces errors
Medical billing and coding regulations change every now and then and keeping up can be very challenging. A Sermo pediatrician commented “As a private practice it is very hard to keep track of billing, all the new rules and have sufficient personnel to do all of that. Unfortunately it does have to be outsourced for us.”
With the constant changes, billing errors are likely to occur. These errors can result in delays in payments, denied claims or being underpaid. The consequences of billing errors can be very expensive. Taking on this task without being up to date on new regulations and policies can result in huge and unwanted expenses.
Billing companies ensure they stay up-to-date on new changes and they also improve their processes to ensure efficiency and minimize errors. Medical coding outsourcing takes off the burden of developing quality assurance mechanisms to ensure compliance with new rules and policies. Furthermore, medical billing companies make use of best-in-class softwares and infrastructure to ensure they maintain accuracy. As a result, they are less likely to make medical billing errors.
4. Increased consistency
Another major advantage of medical billing outsourcing is that it provides staffing consistency. Most in-house medical billing teams are small with only a few people responsible for all coding and billing tasks. Due to the small size of the team, billing activities are prone to workflow interruptions when team members are unavoidably absent. This can be completely avoided with outsource medical billing services.
Third-party billing companies are responsible for processing billing efficiently and are also expected to deliver on-time. They are required to have contingency plans for when staff have to be absent from work. Healthcare organizations can be assured they will receive their payments whether or not someone is out of office.
5. Secured patient data
Medical billing companies are more conscious about data security and compliance concerns. When sharing medical data, a lot of private information is exchanged and it is important to keep these safe from hackers. Billing companies employ up-to-date software and robust data security measures to prevent data loss and other cyber incidents. Outsourcing medical billing ensures that patient data is transmitted safely and securely between providers and payers
6. Increased practice revenue
Outsourcing medical billing can change a practice’s revenue by bringing more revenue and also by speeding up the revenue cycle. Medical billing companies are more efficient in getting claims approved by insurance companies and they can process claims faster. This means less denied claims, more revenue and faster payment collection for healthcare providers.
In sum, by contracting the best medical billing service, healthcare providers can enjoy the dual benefit of increased revenue and faster turnover.
Cons of outsourcing medical billing
1. Lack of control
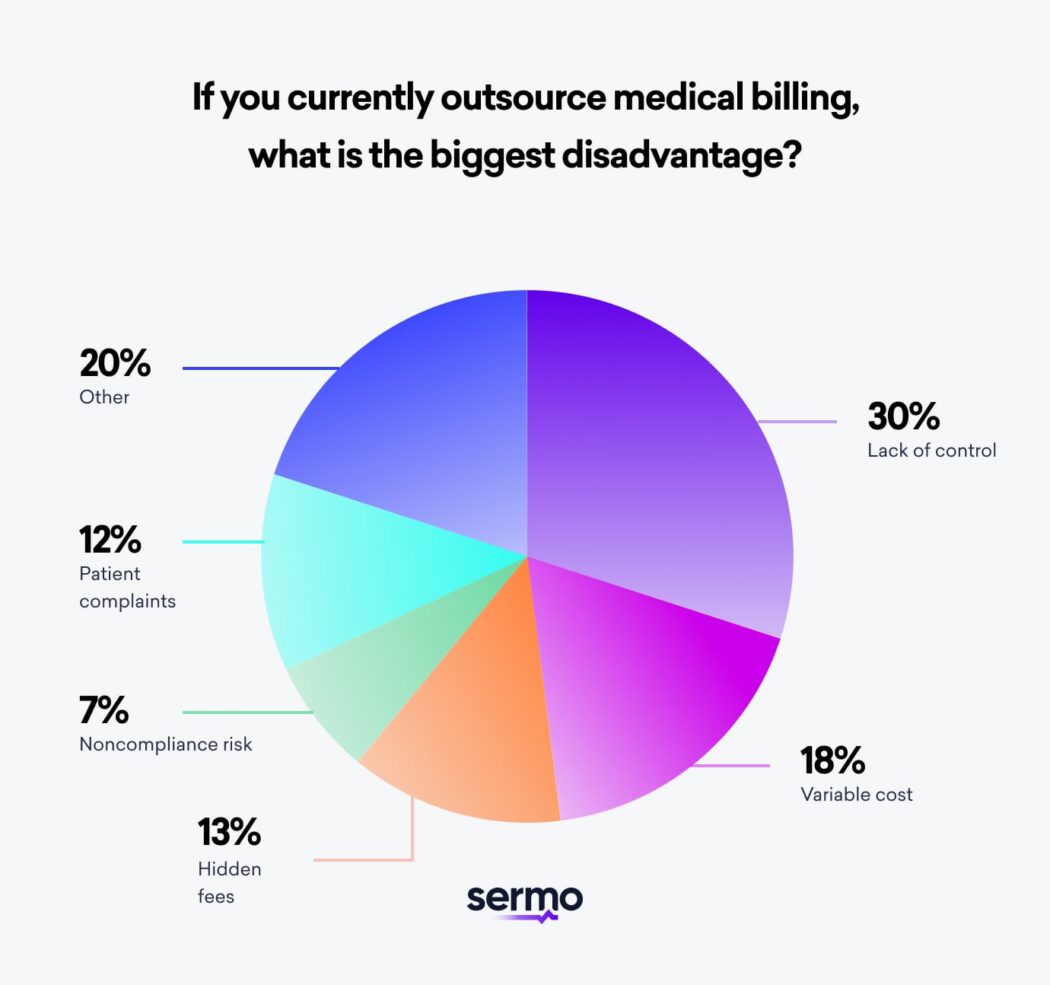
A major concern healthcare organizations have over medical billing outsourcing is the lack of control. In a recent Sermo poll, 30% of physicians indicated lack of control as the biggest disadvantage of outsourcing medical billing. When health organizations contract out their medical billing to a third-party, they have to give up control completely and this can be uncomfortable for hands-on managers.
Giving up this control also means that external billing companies may choose to prioritize highest value accounts to increase their revenue potential. In addition, medical billing companies also handle customer care and this may be an issue especially for patients who aren’t comfortable with a third party accessing and processing their data and accounts.
2. Variable costs
Another downside to medical billing outsourcing is the non-fixed costs. Most billing companies charge a percentage of all payment collections which means more charges with more pay-outs. A Physician in Medicine & Rehabilitation shared on Sermo, “Outsourcing billing is expensive at 6-8% of collections. This is the main issue especially if the office staff can be kept busy doing it.”
3. Hidden fees
There may be hidden fees that come with outsourced medical billing services and healthcare providers should be aware of this. Transferring to an external billing setup can have significant cost implications in the early stages. Extra costs may pop up for upgrading infrastructure, startup charges, membership fees, legal fees, etc. This can be even more challenging for standalone clinics, rural outpatient clinics, small medical centers, and private physicians.
4. Risk of noncompliance
Because medical billing is out of your control when contracting external billing companies, risk of noncompliance can be a concern. Furthermore, cyber attacks and security challenges can put your patient’s private information at risk. Before selecting a medical billing company, it is advised to confirm your partner is HIPAA compliant and has security protocols in place to protect patient privacy.
5. Inconveniencing patients
By outsourcing medical billing and giving consent to third party companies to contact patients on your behalf, there could be risk to patient patients’ satisfaction. Some patients prefer settling their payments directly with in-house staff of the hospital and may feel uncomfortable being contacted about payment by an external party.
In a Sermo poll, 12% of physicians indicated patient complaints as the biggest disadvantage of using medical billing companies.
6. Lack of flexibility
One major advantage in-house billing has over outsourced billing services is the flexibility. With an in-house team, billing practices can be better controlled, communication can be easier and workflow can be adjusted and productivity increased to meet specific time-bound goals. Basically, an in-house team can be more flexible to meet set targets. Unfortunately, this can not be said for outsourcing medical billing services.
Is outsourcing medical billing right for your practice?
This remains a puzzling question for many health practitioners. As one of the US-based Pediatrics physicians states in the comments of a recent Sermo poll, “these are the difficult decisions that us M.D.’s have to make nowadays. Each practice has to decide what is best for them.”
Deciding to outsource has amazing benefits but one must consider the cons as well as the needs and structure of the health organizations. We have a first-hand account from a Sermo Medical Advisory Board member and Infectious Disease specialist, Claudia Martorell, MD, MPH, FACP, who has used both in-house billing and outsourced medical billing services. She shared with us the reasons for the choice and the needs of her organization.
“Currently I have a biller on site. However, I have outsourced medical billing in the past when the previous practice biller resigned due to personal health related reasons. When that happened, I had to quickly look into options of either getting another biller onsite versus outsourcing medical billing. I looked into practice management help options including my region’s medical society and Sermo. I thought they were both helpful in different ways: one helped in providing recommendations of reliable billing companies in the area to work with; the other platform helped in getting feedback on the benefits vs risks of in-house billing vs outsourcing billing. I also learned on the platform about other management tips.
Outsourcing medical billing was the best option at that particular point in time when I needed to be able to work with a stable and reliable company and know that the job was going to be done; however, even though I think the practice had less control over claim denials and reimbursements, it was what the practice needed at that time.
An in-house Biller is what is needed right now; The communication is better with the staff and the in-house biller in terms of coding, billing, submitting denials, and insurance verifications, so I do feel the size and relationship with the billing company matter in terms of maximizing revenue. I have learned that the percentage pricing model is negotiable and varies depending on the company or biller you work with.”
There are no hard and fast rules for picking your medical billing method but every practice must choose a method carefully. If you are still wondering if outsourcing is right for you and perhaps you need to hear more about the experience of other healthcare practitioners, you learn from other physicians with real-life experiences on Sermo. Connect with other physicians on Sermo and join the conversation on medical billing by signing up today.