By 2040, the number of new cancer cases per year is projected to rise to 29.5 million, with cancer-related deaths expected to reach 16.4 million globally.1 These staggering statistics underscore the need for effective treatments, including neoadjuvant therapies, which play a vital role in breast cancer care.
When comparing neoadjuvant vs adjuvant therapy, neoadjuvant therapy is administered before surgery to shrink tumors, halt disease progression, and improve surgical outcomes, while adjuvant therapy is delivered post-surgery to eliminate residual cancer cells and reduce the risk of recurrence.2
Doctors inside Sermo’s exclusive physician community were asked about their priorities when selecting neoadjuvant therapies; responses revealed the following:
- 68% prioritize regaining control of the disease
- 18% focus on improving the patient’s quality of life
- 11% emphasize the urgency to overcome resistance3
So, what therapies do Sermo members use? How do they decide, manage side effects and stay informed on the latest advancements? This article leverages insights from the Sermo community to provide answers.
Neoadjuvant therapy for cancer: when and how physicians use it

Overview of neoadjuvant therapies
Neoadjuvant therapies aim to shrink tumors, improve the success of surgery, and sometimes allow for less invasive procedures. These treatments can also assess how the cancer responds to specific therapies, guiding further treatment plans.2
Key neoadjuvant therapy types include:
- Chemotherapy
- Immunotherapy
- Hormone Therapy
- Targeted Therapies4
Sermo physicians consider several factors when choosing a therapy, including:
- Patient-centered factors: One physician notes, “Management should always consider tolerability and lifestyle fit.5”
- Clinical trial opportunities: An internal medicine physician on Sermo shares, “Improved survival in resectable cancers often stems from neoadjuvant clinical trials.5”
- Research-driven innovation: Another physician highlights the need to “strengthen scientific research and accelerate its translation into public policies.6”
Physicians on Sermo emphasize a patient-centered approach when selecting therapies, prioritizing factors like tolerability and lifestyle fit. They also value participation in clinical trials and advocate for research-driven innovations to improve survival rates and influence public health policies.
Types of neoadjuvant therapies

Chemotherapy in neoadjuvant therapy
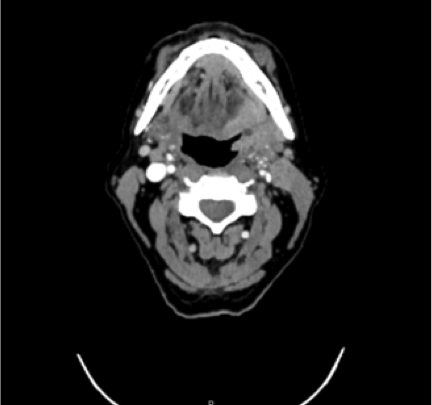
Neoadjuvant chemotherapy for breast cancer remains a cornerstone of treatment, particularly for aggressive cancers like triple-negative breast cancer (TNBC) and other challenging tumor types. By targeting rapidly dividing cancer cells, chemotherapy reduces tumor size, often enabling less invasive surgeries and providing key insights into tumor response. Moreover, it addresses micrometastases early, potentially lowering the risk of recurrence.7
The physicians on Sermo frequently discuss chemotherapy’s role in forums like the NEOSTAR trial findings for resectable non-small cell lung cancer (NSCLC). For instance, participants in the trial achieved a major pathologic response (MPR), defined as 10% or less residual viable tumor (RVT) at surgery.8 These findings, shared in the Sermo community, highlight chemotherapy’s evolving use alongside immunotherapy in modern oncology. Sermo members note that such discussions are invaluable for understanding treatment efficacy and enhancing clinical decision-making.5
However, doctors on Sermo emphasize balancing chemotherapy’s effectiveness with its side effects — such as fatigue, nausea and immunosuppression — is critical.5 Insights shared in the community underscore its transformative potential when combined with other therapies but also highlight the need to manage patient quality of life throughout treatment. These discussions not only share knowledge but foster collaboration on ways to optimize patient outcomes using neoadjuvant chemotherapy.
Neoadjuvant immunotherapy
Immunotherapy is transforming neoadjuvant treatment, particularly for triple-negative and HER2-positive breast cancers, by enhancing the immune system’s ability to target cancer cells. A study by the Cancer Research Institute highlights advances in targeted antibodies, like trastuzumab (Herceptin®) and pertuzumab (Perjeta®) and checkpoint inhibitors, such as pembrolizumab (Keytruda®), which show significant benefits for PD-L1-positive TNBC.9
However, challenges persist, including managing side effects like fatigue, rash and inflammation, as well as resistance in some patients.
A Sermo endocrinologist emphasized any treatments should try to reduce the impact on a patient’s gut microbiome, describing it as “an essential organ that maintains a vital dialogue with our immune system, supporting immune balance and function.5”
This link underscores the importance of maintaining gut health through lifestyle adjustments and supportive care to optimize immunotherapy outcomes and reduce adverse effects.
Hormone therapy in neoadjuvant therapy
Hormone therapy is a critical component of neoadjuvant treatment for hormone receptor-positive (HR+) breast cancers.10 By blocking the cancer’s access to estrogen or progesterone, it slows tumor growth and can shrink tumors prior to surgery.
According to poll results, oncologists on Sermo adopt different strategies when first-line therapies fail. 55% prefer switching to another doublet regimen, often combining hormone therapy with agents like CDK4/6 inhibitors. 28% choose to change therapy classes while maintaining combination regimens, and 10% intensify treatment by adding a third agent.3
While hormone therapy is generally well-tolerated, its slower action compared to chemotherapy may not be ideal for rapidly growing tumors.
Which targeted therapies in neoadjuvant therapy are best?
Targeted therapies provide precision treatment by addressing specific molecular pathways in breast cancer. For patients with HR+HER2- breast cancers, especially those with PI3K mutations, these therapies are a significant advance.
Doctors in the Sermo community show a preference for the following targeted agents:
- Capivasertib (61%): An AKT inhibitor favored for its efficacy and tolerability.
- Alpelisib (18%): A PI3K inhibitor effective for PI3K-mutant cancers but limited by side effects like hyperglycemia.
- Everolimus (14%): An mTOR inhibitor addressing downstream pathways, though concerns about stomatitis and fatigue reduce its use.3
For PI3K wild-type tumors, Alpelisib (39%) and Everolimus (36%) remain leading choices, with Capivasertib (21%) also being considered.3 While these therapies hold great promise, oncologists must navigate side effects and resistance mechanisms to maximize patient outcomes.
Physicians’ patient management considerations

Managing patients with HR+HER2- advanced breast cancer that’s progressed on first-line (1L) therapy requires careful deliberation to address both clinical and patient-centered priorities. Insights from a Sermo oncology poll highlight the primary goals oncologists aim to achieve in such cases.
The most significant priority, cited by 68% of oncologists, is regaining control of the disease.3 This involves halting tumor progression and restoring responsiveness to therapy to improve patient outcomes.
For 18%, the focus shifts to maintaining the patient’s quality of life,3 emphasizing the selection of treatments that minimize side effects and align with individual lifestyle needs.
Meanwhile, 11% of oncologists on Sermo emphasize the urgency of overcoming resistance to initial therapies and exploring innovative solutions to counteract treatment failure.3
This data reflects the nuanced decision-making oncologists must employ. Balancing disease control with patient comfort and addressing therapeutic resistance often leads to a reliance on second-line options, including targeted therapies, hormone therapy combinations, or novel agents. The choice of therapy depends on tumor biology, prior treatment response and patient tolerance.
Ultimately, oncologists strive to tailor interventions that balance efficacy with quality of life, underscoring the complexity and importance of individualized care in managing advanced breast cancer.
Emerging trends and future directions
Neoadjuvant therapy is advancing rapidly, with innovations like immunotherapy showing significant potential for improving outcomes in advanced breast cancer. Clinical trials are a focal point, according to many doctors on Sermo – with one noting, “The study of cases in oncology is of utmost importance.11”
Physicians play a vital role in advancing these treatments. According to a Sermo poll of its members, 63% of surveyed physicians have participated in cancer research studies and 69% expressed interest in contributing to or conducting research, ensuring therapies address real-world challenges.12
How to keep up with emerging cancer therapies

- Stay Informed with Research: 73% of physicians in the Sermo community look up cancer treatment research weekly and 52% rely on medical journals.12 One Sermo member noted, “We must study new treatments daily. Human intelligence together with development and artificial intelligence can win the battle against this dreaded disease.13”
- Leverage the Power of a Global Community: Participate in peer discussions, including exclusive Tumor Board cases, to exchange insights and tackle complex issues. As an example, one oncologist on Sermo recently sought advice on sequencing neoadjuvant chemoradiation for a 74-year-old patient with rectal cancer, sparking valuable shared learning.14
- Participate in Medical Research: Provide feedback via paid surveys for doctors on topics like patient challenges (such as access and affordability) and specialized clinical interests to influence health policies and improve cancer care delivery.
- Engage with Leading Conferences: ASCO is a top educational event attended by 79% of surveyed oncologists. Key sessions include education (70%), oral abstracts (54%) and clinical symposia (42%), with 39% attending virtually in 2023.15
- Adopt Advanced Technologies: AI and CRISPR are revolutionizing diagnosis and treatment, improving early detection and enabling personalized care.
- Collaborate with Networks: Alliances with organizations like ASCO foster advancements in oncology. A Sermo member emphasized, “Union among professionals is key to developing better protocols.15”
- Invest in Administrative Support: Hiring paralegals streamlines case management and research logistics, allowing more focus on clinical care.
Your takeaway
Neoadjuvant therapies are essential in modern breast cancer treatment, addressing tumor shrinkage, disease progression and surgical outcomes.
Sermo insights reveal that 68% of oncologists prioritize disease control, while 18% focus on quality of life and 11% on overcoming resistance.3
Innovations like immunotherapy, targeted therapies and hormone combinations are reshaping care, with 63% of physicians participating in research and 73% reviewing cancer advancements weekly.12
Personalized, informed approaches remain key to improving patient outcomes.
Join the conversation on Sermo
Connect with thousands of physicians worldwide, including more than 400k in the US alone, and gain exclusive insights into the latest advancements in cancer care. Collaborate on challenging cases, participate in impactful research, and share your expertise to shape the future of oncology.
Footnotes
- National Cancer Institute (NCI), 2024. Cancer Statistics
- Cancer Treatment Centers of America
- Sermo, 2024. Poll of the Week: How Do You Manage Treatment for HR+/HER2- Advanced Breast Cancer Patients?
- National Cancer Institute (NCI), 2024. Neoadjuvant therapy
- Sermo member, 2024. Comment on Major pathologic response in trial of patients with resectable NSCLC.
- Sermo member, 2024. Comment on Physicians Are Indispensable to Cancer Research.
- Mayo Clinic
- Sermo, 2024. Major pathologic response in trial of patients with resectable NSCLC.
- Cancer Research Institute
- National Cancer Institute (NCI), 2024. Hormone Therapy for Breast Cancer Fact Sheet.
- Sermo member, 2024. Comment on Advancing Cancer Care—the 2021 ASCO Annual Meeting.
- Sermo, 2024. Cancer Treatment & Research.
- Sermo member, 2024. Comment on Physicians Are Indispensable to Cancer Research.
- Sermo member, 2024. Comment on Tumor Board – Total Neoadjuvant for Rectal.
- Sermo member, 2023. Comment on 2023 ASCO Annual Meeting—Will You Be There?