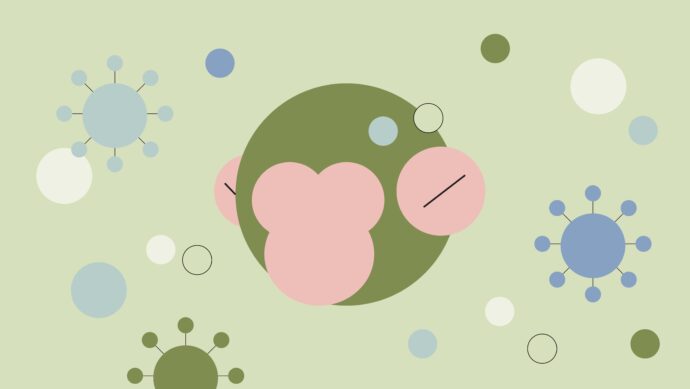
In 2024, the Mpox virus outbreak—formerly monkeypox—continues to demand the attention of Doctors around the globe1. Earlier this year, Africa’s top public health body announced the virus to be spreading quickly, with more than 17,000 suspected cases and more than 500 deaths2.
The World Health Organization (WHO) recently reclassified the disease as a public health emergency following new outbreaks across the Democratic Republic of the Congo and neighboring countries1. The disease has evolved from a regional concern to an issue with potential global implications, such as increased occupancy in hospitals and longer waiting times for patients. WHO Director-General Dr. Tedros Adhanom Ghebreyesus notes, “A coordinated international response is essential to stop these outbreaks and save lives1.”
Physicians in the Sermo community are taking the possibility of a wider Mpox outbreak seriously. Despite the fact that only 19% of surveyed doctors have seen Mpox cases in their own practices, 51% believe Mpox could reach pandemic status if unchecked3.
What’s driving these concerns and how can Doctors work to mitigate the threat? This article explores the perspectives shared by the Sermo community on what physicians need to know and the proactive steps that can make a difference.
What is Mpox?
Overview of the Mpox virus
Mpox is caused by the monkeypox virus, part of the Orthopoxvirus genus, which also includes smallpox.
The virus has multiple variants or clades, each with different transmission rates and severity. The new Mpox strain, Clade I, including subclades Ia and Ib, is driving new outbreaks, spreading easily through close contact, which makes awareness crucial for Doctors1.
Mpox Primarily Spreads via:
- Skin-to-skin contact
- Respiratory droplets
Putting individuals with close personal contact, such as those with multiple sexual partners, at higher risk.
Vulnerable Groups Include:
- Healthcare workers
- Immunocompromised individuals
- Children
Given that as of 2023, the CDC reported less than 23% of US residents within high risk groups were fully mpox vaccinated, more needs to be done to spread awareness and safeguarding measures4.
How has the Mpox resurgence affected doctors’ practices in 2025?

Regional differences in physician approaches to Mpox
Physician experiences with monkeypox treatment and cases have varied widely, depending largely on geographic location.
In some regions, physicians haven’t encountered the disease at all. One US-based Sermo member specializing in Emergency Medicine reported, “In my area of the country, we’re not seeing cases, and there’s a general lack of awareness5.”
Conversely, in regions like Africa, where Mpox is more common, there’s a heightened level of concern. “I’m deeply concerned, especially for the health and well-being of children at risk of the Mpox virus, which is spreading quickly in Africa and beyond5,” shared an Anesthesiology Sermo community member.
Given the high rate of international travel, doctors caution against viewing Mpox solely as a regional disease or a disease that only affects specific communities.
What are the top challenges doctors face with Mpox?
From identifying the disease to preventing its transmission, Mpox presents unique challenges for doctors.
Identification

One of the primary obstacles in diagnosing monkeypox symptoms is the fact that the virus can resemble those of other common infections, such as chickenpox or herpes.
According to a Sermo poll, 46% of physicians see distinguishing Mpox from these similar conditions as the main diagnostic challenge3. A Family Medicine / Practice Sermo member added, “The Monkeypox outbreak highlights the need for more awareness and specialized training for HCPs, mostly in early detection5.”
From the Zika virus outbreak, we can learn the importance of accessible, local testing options. During the Zika outbreak, “59% of 2,241 U.S. doctors [thought] that lab tests for Zika Virus should be available at local/state public health laboratories in addition to the Centers for Disease Control (CDC)6,” and similar infrastructure could improve Mpox detection.
Transmission
Prevention of Mpox transmission remains challenging, with 36% of Sermo physicians identifying it as a significant hurdle3. Because the virus can spread through close contact, clinics, hospitals and other high-contact settings are particularly susceptible to outbreaks.
Looking back at Zika, physicians observed that a broad approach to travel warnings was helpful. Then, 68% of 4,085 global doctors thought that travel warnings should be extended beyond pregnant women to include all women of fertile ages6.
Adopting inclusive travel advisories for high-risk groups could similarly reduce Mpox spread among vulnerable populations.
Health authority involvement and communication
According to the Sermo poll, 86% of physicians believe health authorities should be more proactive in pandemic prevention3. One US-based Pediatrics Sermo member shared, “The government’s lack of investment in raising awareness about monkeypox is a glaring failure in public health policy5.”
Reflecting on COVID-19, many physicians felt that delayed government communication led to slower frontline responses. Then, many Sermo members believed the state and government actions weighed public and economic concerns, but faster, more transparent communication was needed7.
Increased clarity from health authorities on preventive actions, symptom awareness and resources would support a more unified response to Mpox.
What are the current discussions around Mpox prevention strategies?

Learning from COVID-19 and Zika
Rapid information sharing and physician collaboration
One key insight from the COVID-19 response was the benefit of real-time physician collaboration.
“Physicians should have more of a voice in how we deal with this pandemic and be able to quickly share information with one another and the world7,” said Peter Kirk, CEO of Sermo.
Community discussions on Mpox, like those within Sermo, could help identify symptoms, report new cases and provide mutual support, allowing for swift insights and responses.
Preparedness for secondary outbreaks and long-term resource needs
Learning from COVID-19, where 83% of global physicians anticipated a second wave7, there’s a clear need for sustained resource planning. A Sermo poll identified PPE, Rapid testing kits, and ventilators as top resource needs7, emphasizing the need for emergency stockpiles for future infectious diseases. An equitable distribution of resources could ensure that underserved communities have timely access to critical support.
Overcoming stigma and misconceptions
Stigma has posed challenges for other viruses, and Mpox is no different.
During the Zika outbreak, a physician observed, “Until the information we have is accurate, the chances of fear-driven overreaction may be justified6.”
In the Mpox context, a GP Sermo member reported that “suspected cases face stigma, leading to stress and isolation5,” and this stigma affects not only patients but also specific communities.
“Some people think it’s only a problem in the LGBTQ+ community5,” shared a Sermo member specializing in Radiology.
Accurate, inclusive communication can help reduce stigma and enable individuals to seek timely care without fear of judgement.
Patient management changes in 2025

As Mpox spreads, many physicians in the Sermo community have shared strategies for addressing patient concerns. A GP member noted, “Many patients are worried about symptoms like rashes and fever, fearing monkeypox5.”
In response, there is a shift toward proactive and supportive care:
- Cautious diagnosis
- Early isolation of suspected cases
- Symptom management
- A focus on hygiene practices
- Targeted monkeypox vaccine use
Physicians are encouraging symptom monitoring in high-risk patients and educating communities about prevention4.
However, several members noted a lack of patient education resources. “Without proper education and resources, communities remain vulnerable, leading to preventable outbreaks5,” warns a Pediatrics Sermo member.
To strengthen response efforts, patient information needs to be easily accessible and accurately communicated.
Public health considerations from the Sermo community
Physicians on Sermo are voicing long-term concerns regarding Mpox.
As WHO declares Mpox a public health emergency for the second time, many feel the need for greater public health investment and support for those on the front lines.
Comparisons with COVID-19 and Zika indicate that containment and effective communication are vital for managing Mpox, with public health education identified as a crucial area for improvement.
Ultimately, the main change in approach that Sermo members urge is for the healthcare community to be proactive in communicating internally with each other and externally with the public. “To control the spread of the disease, more epidemiological information must be provided to the population5,” notes a GP member, emphasizing the role of education in outbreak prevention.
Continue the Mpox discussion: Join the Sermo community

The Sermo platform offers an invaluable space for physicians to discuss, share, and learn from one another. Continue the Mpox discussion here and connect with peers on topics that matter to you.
Sermo empowers you with:
- Community-driven insights and expert opinions
- Real-world data from live polls
- Shared experiences of physicians worldwide
Join the conversation today to stay informed, supported, and ready to tackle emerging health challenges.