Meaningful use in healthcare is an integral element in advancing patient care and improving IT security. The US government introduced the Meaningful Use Incentive Program in 2009 as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act1. Yet, despite its longevity, our recent survey of over 100 physicians revealed that only 54% have a clear understanding of the Meaningful Use Program. (If this is you, find out, go directly to How to meet meaningful use criteria)
“Like everything, there is a learning curve before it becomes useful.”
Hematology Oncology, Canada
If you’re one of the remaining 46% of physicians who feels unclear on the meaningful use medical definition or what the program means for your practice, we’ve compiled this quick guide to help fill in the blanks.
What is meaningful use in healthcare?
Let’s start with the basics: what is meaningful use, and why is it important?
If your practice provides care for Medicare or Medicaid patients, you already know that the government has taken an increasingly focused stance on streamlining the way we deliver care in recent years to emphasize quality over quantity. Hence the introduction of the meaningful use in healthcare program.
The definition of meaningful use refers to the adoption of the Centers for Medicare and Medicaid’s (CMS) electronic health record (EHR) to improve efficiency, safety, data security, and outcomes. Physicians should be using technology in a meaningful way to improve patient care. In our survey, 84% of physicians globally said they currently use EHR in their practices, hospitals, and clinics.
“In my country, everything is computerized, and this is a wonderful resource for accessing all patient information immediately and being able to coordinate specialties.”
Urology, Spain
“Useful in order to keep data and create networks among different professionals.”
Psychiatry, Italy
In the US, healthcare providers using certified electronic health records technology (CEHRT) are eligible for financial incentives of between $44,000 (Medicare) and $63,750 (Medicaid).
However, there is still some debate over the effectiveness of EHR practices. Some of the negative sentiment towards meaningful use in healthcare is likely due, at least in part, to the fact that the meaningful use definition in the US also includes the 2017 addition of penalty schemes for non-compliance.
“While I fully support the use of EMR and would never go back to paper, Meaningful Use is meaningless and functions only as a mechanism for fines and penalties. I have opted to take the Medicare cuts rather than risk the potential fines.”
Neurosurgery, US

The pillars of meaningful use
CDC guidelines define meaningful use in relation to five specific pillars of health outcomes:
- Improving quality, safety, and efficiency while reducing health disparities In our survey, 50% of physicians said they considered this the most important factor.
- Improving care coordination
The second most popular physician factor, with 25% of physician votes. - Improve public health
Rated the most important by 9% of doctors. - Engaging patients and families
The most important factor to 8% of physicians. - Ensure privacy for personal health information
The most significant consideration for 8% of the physicians in our survey.
The history of meaningful use: the three stages
To gain a deeper understanding of meaningful use in healthcare, it helps to look at the history and development of the program, and where it stands today. The government rolled out a staged implementation system to provide healthcare facilities and professionals adequate time to adopt and integrate new EHR and e-Prescribing systems.
Stage 1 – 2010
Stage 1 emphasized certified EHR adoption, proper electronic data capture, and more efficient data sharing. Healthcare providers were able to receive incentives based on meeting core objectives. At the time, some of the most relevant benchmarks for eligibility included being capable of:
- Processing 40% of prescriptions electronically using a certified EHR process.
- Submitting electronic data to immunization information systems or registries.
- Submitting electronic data as required by local and practice regulations.
- Submitting electronic data on lab results to public health agencies.
- Submitting syndrome surveillance data to public health agencies electronically.
Stage 2 – 2012
Stage 2 increased the thresholds for compliance, documentation, and improved clinical processes. For example, the threshold percentage for electronically processed prescriptions rose to 50%. Additional criteria were also introduced concerning:
- Decision support
- Care coordination requirements
- Patient engagement rules
During this stage, particular focus was placed on developing the capability to identify and report various cancer and other specified cases to state and special registries.

Stage 3 – 2014 to 2017
In the final stage of implementation, the focus moved towards higher levels of interoperability and improving patient outcomes. The list of qualifying criteria was significantly extended to include:
- Protecting patients’ PHI by completing a security risk analysis of EHR software.
- Enabling checks for drug-drug and drug-allergy interactions.
- Implementing five clinical decision-support interventions relating to no less than four clinical quality measures (CQMs).
- Using a Computerized Provider Order Entry (CPOE) to order at least 80% of medication orders, and 60% of lab orders and diagnostic image orders.
- Activating patient portal features to enable patients to access their own electronic health information.
- Demonstrating coordination of care by improving patient engagement.
- Creating electronic summary of care records for health information exchange transfers.
- Meeting three out of five public health and clinical data registry report requirements (across immunization, syndromes, case reporting, public health registries, or clinical data registries).
In 2017, we also saw the introduction of the meaningful use penalty, meaning physicians now receive reduced Medicare reimbursements in the event of non-compliance with key criteria.
So, precisely what is meaningful use in today’s physician environment? And where does your practice stand? You can find a comprehensive list of objectives on the CMS website, although it’s essential to note that the requirements for individual practitioners and hospitals differ significantly.
Why is the Meaningful Use Incentive Program important?
Poorly designed and implemented EHRs leave patient personal health information (PHI) open to data breaches and fraud. Plus, they have the potential to lead to errors in medication and treatment, etc. When used effectively, EHRs and e-Prescribing software streamlines workflows while simultaneously protecting patient data, allowing you to provide a higher standard of care and improve patient outcomes.
“I think the use of EHR can facilitate health services significantly. Therefore, such a system can be of significant importance to our daily practice.”
Cardiothoracic Surgery, Great Britain
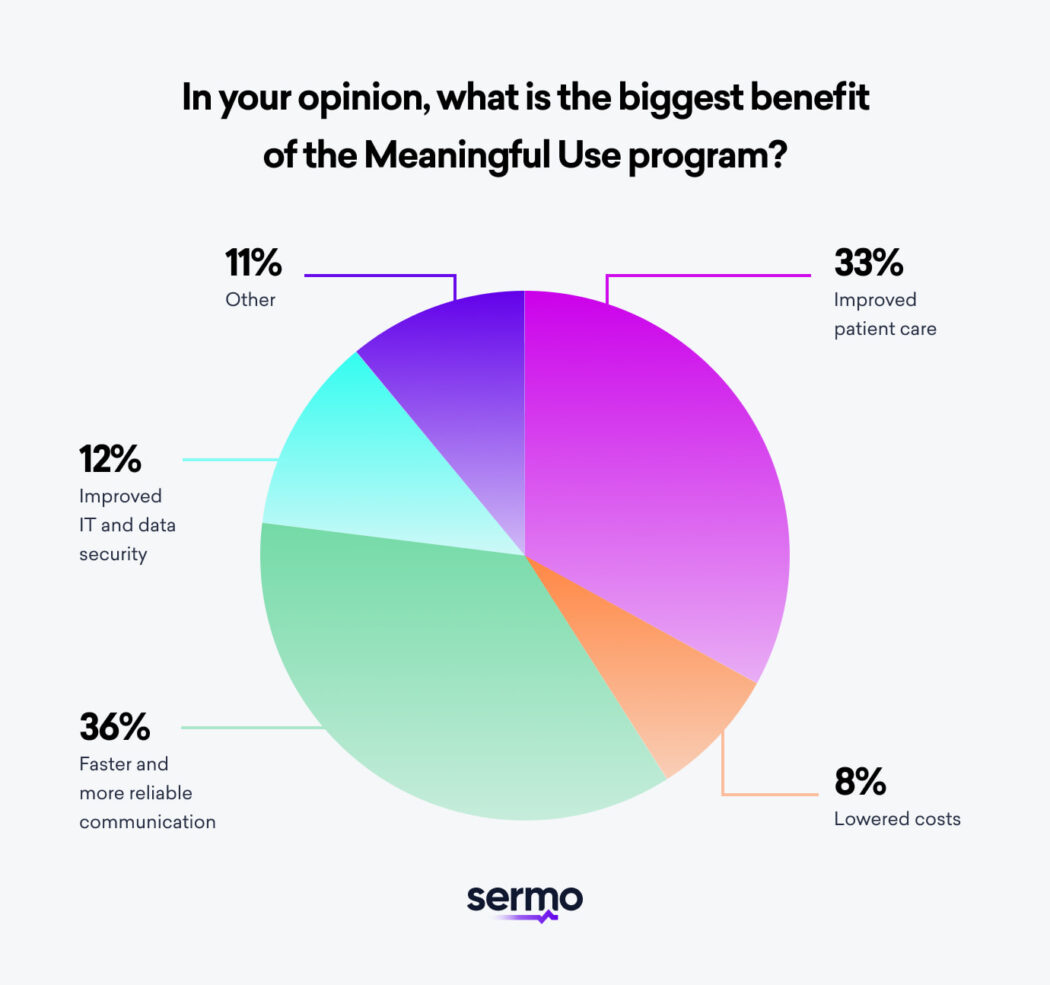
But, more specifically, what does meaningful use mean to you and your practice, hospital, or clinic? According to our survey, the most significant single benefit of meaningful use in healthcare is:
- Faster and more reliable communication – 36%
- Improved patient care – 33%
- Lowered costs – 8%
- Improved IT and data security – 12%
- Other – 12%
Challenges of the Meaningful Use Program
While most physicians are keen to comply with all stages and meet the newest 2017 criteria, that doesn’t mean the transition has been straightforward. The physicians we surveyed cited several challenges, the most significant being:
- Cost of implementation (30%)
“Documenting that requirements are being met and doing the required reporting takes time and costs which are not reimbursed adequately even considering the so-called incentives.”
Cardiology, US
- Lack of integration with existing systems (21%)
“Data sharing is still a problem since different practices and health systems use different companies that don’t talk to each other.”
Obstetrics & Gynecology, US
- Training staff (15%)
“Although EHRs improve patient flow and retrieval of medical information, it is time-consuming and an administrative burden.”
Pediatrics, US
- Workflow changes (14%)
“There is little that’s more frustrating in daily workflow than EHR. It holds great promise but until now has NOT delivered.”
Obstetrics & Gynecology – Reproductive Endocrinology & Infertility, US
- Lack of interoperability (8%)
“EHR would help saving so much time, costs, space (paper!!!) and it’s just nonsense that still no full interoperability is available!”
Emergency Medicine, Italy
- Low-quality data and reporting (7%)
“The ease of data collection possibly offsets the time I spend (waste) messing with the computer. Not sure which side is the winner yet.”
Anesthesiology, US
- Privacy concerns (5%)
“There are concerns about patient’s and data privacy, safety, and security.”
Pediatrics, US

How to meet meaningful use criteria
How can modern-day physicians ensure compliance? Here are a few suggestions on how you and your practice, clinic, or hospital can work toward meeting the meaningful use criteria:
- Verify that the EHR system you use is certified by checking with your vendor or the Office of the National Coordinator for Health IT (ONC) website.
- Introduce electronic prescribing of controlled substances (EPCS) to your clinical workflow to increase your e-Prescribing numbers and simultaneously improve fraud protection and patient satisfaction.
- Invest in single sign-on technology to improve your clinical workflow through more efficient user-switching, work-station sharing, and authentication management.
- Conduct an annual security risk review and analysis as per HIPAA and Meaningful Use requirements.
- Apply for a hardship exception per American Medical Association recommendations to ensure you can still receive incentives, even if you have not fully met the criteria.
Power up your practice with Sermo
Still unsure about meaningful use definitions and best practices? Sign up for a Sermo account and start building a global professional network where you can access all the information and professional advice you need.