94% of physicians believe that empathetic care improves patient outcomes, yet nearly half (47%) feel that traditional medical training limits their ability to connect emotionally.1
This conflict underscores broader cancer care ethical dilemmas, from balancing cutting-edge treatments with quality of life to addressing disparities in access and affordability.
How can oncologists and other physicians navigate these complex ethical issues in cancer treatment? What steps can they take to align technological progress with the compassionate care patients with cancer deserve?
Drawing from the insights of oncologists and other physicians on Sermo, this article explores the ethical concerns in oncology today and highlights actionable strategies to address them.
Ethical dilemmas in cancer care
What are the biggest ethical issues in cancer care?

Balancing aggressive treatments with quality of life
Cancer care presents physicians with complex ethical challenges, particularly in balancing aggressive treatments with patient quality of life and in balancing cancer care with patient autonomy.
For terminal patients, aggressive interventions may extend life but often come at the cost of physical and emotional well-being. Physicians must navigate these decisions by empowering patients through clear, honest communication that aligns treatment plans with their values and goals. As a General Practice Sermo member notes, “Without pain, the rest of the fears related to cancer can be faced in a more positive way.2”
Public education and awareness
Public education also plays a pivotal role, particularly in countering misinformation. Parental refusal of HPV vaccines due to misconceptions highlights the need for proactive campaigns. “More needs to be done to discredit websites that promote false information about this vaccine,3” emphasizes a doctor on Sermo who works with pediatric patients.
Misinformation and lack of public awareness are leading to delays in diagnosis and treatment. One US-based Oncologist on Sermo poignantly suggests that “the only thing we can do to increase early diagnosis is to invest in good US radiologists and awareness advertisements for patients.4”
Raising adequate public awareness and preventing widespread misinformation around cancer care demands a patient-centered, ethically grounded approach to ensure equitable, compassionate care.
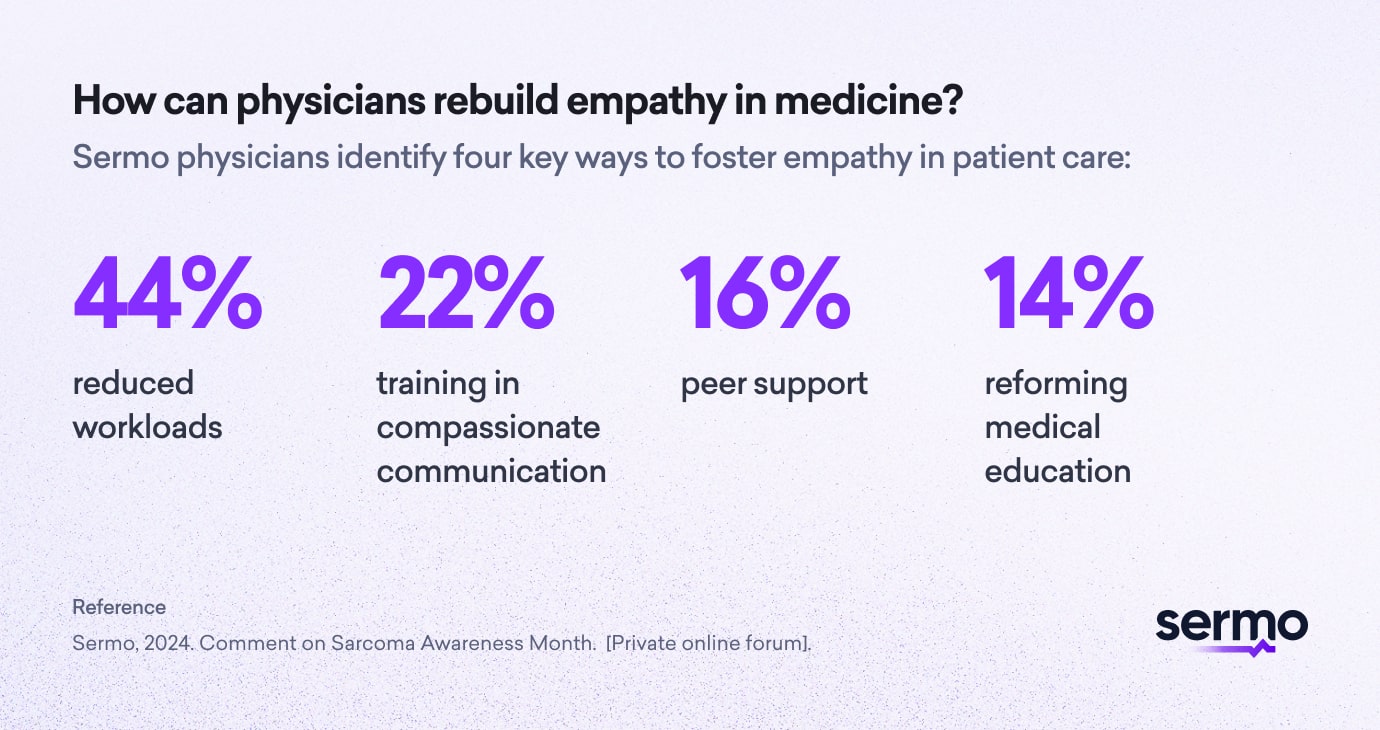
Barriers to compassion in modern medicine
Empathy and compassion are foundational to effective patient care, with 94% of physicians agreeing that patients respond better to empathetic care. However, 47% of doctors believe traditional medical training hinders emotional connection, while 70% express concern about the impact of suppressing vulnerability in patient interactions.5 This conflict underscores the barriers preventing physicians from fully embracing compassion.
As one doctor on Sermo observes, “The lack of education in empathy1” further compounds these challenges. Furthermore, emotional exhaustion and burnout, cited by 78% of physicians, leave many unable to engage with patients at their best.6
The consequences for patients are significant. Detached care erodes trust, creating a sense of indifference and isolation. “By showing empathy, they could feel that someone they trust is advising them,1” notes a Dermatologist Sermo member. Poor communication and diminished adherence to treatment plans are common outcomes, while impersonal interactions weaken therapeutic relationships.1
As one Internal Medicine physician emphasizes, “The doctor-patient relationship should not be blown under any circumstances.”
Disparities in screening and treatment: Addressing inequities in cancer care
Disparities in cancer care remain a critical challenge, driven by socioeconomic, geographic and systemic inequities.
According to Sermo members, these barriers limit access to treatment (20%), diagnostics (12%) and essential resources, such as HPV vaccinations, which are often unaffordable for many. Financial challenges (23%) compound the issue, while 15% of patients face a lack of education about available care. Geographic barriers, affecting 12%, further isolate rural or remote populations from timely screenings and treatments. Together, these factors impact 18% of all cancer patients.7 One Oncologist on Sermo laments that emerging cancer treatments are less readily available to patients “across poorer nations8.”
The consequences are severe. Patients often experience advanced-stage diagnoses due to delayed care, contributing to higher mortality rates. Psychological stress from these inequities adds to the burden on patients and their families.
For women, the lack of access to HPV vaccines is particularly devastating, leading to preventable deaths. “The HPV vaccine is placed in our country, but its high cost means not everyone can access it,3” a pediatrician notes.
Addressing these disparities requires targeted interventions. Expanding subsidized care, improving patient education and establishing government-funded initiatives can close gaps in access. Prioritizing equitable resource allocation, enhancing geographic reach with mobile diagnostics and leaning on community partnerships are essential to ensuring that all patients receive the care they need to improve outcomes and save lives.3

Access to mental health resources
Access to mental health resources remains a significant ethical challenge in cancer care. The psychological toll of a cancer diagnosis often demands professional mental health support, yet many patients face limited access to these vital services. Integrating psychologists or mental health professionals into care teams is crucial for addressing emotional distress and promoting overall well-being.2
Doctors frequently face difficult decisions about resource allocation, having to prioritize care for some patients over others when services are limited. Moreover, navigating cultural and personal resistance to mental health interventions can create conflicts between respecting autonomy and advocating for the patient’s well-being. In such instances, healthcare professionals must navigate the delicate balance between respecting a patient’s autonomy and advocating for their overall well-being.
Providing information about support groups tailored to cancer patients and their families is another essential step. These resources help patients process their diagnosis and navigate the challenges of treatment. As one GP on Sermo emphasizes, “Even for those with no history of mental health illness, a cancer diagnosis is life-changing.2”
Addressing this gap requires doctors to advocate for expanded mental health support, ensuring equitable access to comprehensive care for all patients.
The role of AI in cancer care: ethical challenges
The integration of artificial intelligence (AI) in cancer care offers immense potential but raises significant ethical concerns that must be addressed to ensure equitable and effective use.
Key ethical challenges of using AI in cancer care
- Risk of Over-Reliance on AI
- While AI can enhance early cancer detection, over-reliance risks diminishing clinical judgment. “AI has immense potential… but it cannot replace skilled radiologists,6” highlights an Orthopedic Surgeon on Sermo. Human oversight remains critical to mitigate errors.
- Bias in AI Algorithms
- AI systems trained on incomplete or biased datasets may produce unequal outcomes. As an Internal Medicine member warns, “AI needs to be carefully validated, and we need to really pay attention to the bias it has.6“
- Ethical Use of Data
- Concerns about patient privacy and consent arise as AI relies on vast datasets. “It has good and bad sides; it can easily be used in the wrong format and create chaos, but when regulated and used wisely, it can likely provide some benefit,6” emphasizes a General Surgery Sermo member.
- Balancing Human Expertise and AI
- Ethical dilemmas arise when determining AI’s autonomy. “AI is a tool to be welcomed, but it does not replace the physician’s experience,6” underscores a Psychiatry specialist.
Unregulated AI could depersonalize care, eroding trust and connection between doctors and patients. As an Internal Medicine member stresses, “Too much tendency to replace human value in consultation, AI would only be usable in the case of information, I do not think that the value of physical contact should be replaced.6“
A balanced approach to technology in care, combining AI’s efficiency with human empathy is essential for ethical and patient-centered care.
How physicians address the economic burden of cancer care

How do doctors balance treatment and cost considerations in cancer care?
Cancer care presents a dual challenge for physicians: delivering the best possible treatment while navigating the financial realities many patients face. This “financial toxicity7” impacts treatment decisions and patient outcomes, demanding innovative strategies to balance care quality with cost considerations.
Early identification of financial distress is crucial. When screenings are inconsistent, patients may forego critical treatments. Currently, only 31% of physicians on Sermo actively screen for financial challenges during intake, while 22% rely on self-disclosure, which could miss vulnerable cases.7 Developing standardized screening tools and training care teams to identify subtle signs of financial strain can address this gap.
High treatment costs lead 37% of patients to delay or skip care, with additional burdens including out-of-pocket medication expenses (17%), travel costs for specialized care (13%) and income loss during treatment (20%)7. These financial pressures can force patients to choose less effective treatments or decline care altogether.
Successful interventions by Sermo members include:
- Subsidized medication programs (26%)
- Nonprofit grant programs (28%)
- Government-funded initiatives (22%)
- Financial counseling (36%)
- Offering clear cost estimates (25%)
- Educating patients about available resources (16%)7
These models reduce patient costs and mitigate financial stress while maintaining care quality, though challenges such as funding limitations and geographic inequities persist.
Your takeaway
How do physicians navigate ethical considerations in cancer treatment?
For physicians, navigating the ethical dilemmas of cancer treatment requires balancing technological innovation, patient autonomy and emotional connection. As one GP on Sermo poignantly observes:
“Medical decisions are never easy, even in the simplest and smallest things. I think that in all the things that really matter… starting with our own way of acting is the place where we can take action.8”
From addressing disparities in access to improving psychological support and integrating AI responsibly, physicians must focus on compassionate, patient-centered approaches. By combining ethical decision-making with empathy and innovation, they can build trust, improve outcomes and ensure equitable care for all.
Join the conversation on Sermo
At Sermo, healthcare professionals come together to share insights, debate solutions, and support each other in tackling these dilemmas.
Discover how peers are addressing financial toxicity, improving access to mental health resources, integrating AI responsibly, and fostering compassionate, patient-centered care.
Footnotes
- Sermo, 2024. The challenges doctors face in revealing their human side. Sermo Community [Private online forum].
- Sermo members, 2024. Comments on Bedside Manner – Cancer Care. Sermo Community [Private online forum]. [Accessed 14 January 2025].
- Sermo member, 2024. Comment on 4,290 Women are Predicted to Die of Cervical Cancer in the U.S. in 2020. Sermo Community [Private online forum].
- Sermo, 2024. Comment on Sarcoma Awareness Month. [Private online forum].
- Sermo, 2024. Poll of the Week: The Challenges Doctors Face in Revealing Their Human Side [Dataset 1125116]. Sermo Community.
- Sermo, 2024. Why does cancer treatment remain a luxury in many parts of the world? [Poll results]. Sermo Community.
- Sermo member, 2024. Comment on Day 2—Breast Cancer Awareness Month Promo. Sermo Community [Private online forum].
- Sermo, 2024. Financial Toxicity and Cancer Treatment: How Oncologists Support Patients in Shared Decision-Making. Sermo Community [Private online forum].