The patient-centered care (PCC) framework has raised healthcare standards. It’s grounded in the clinical efficacy of a collaborative partnership between patients and healthcare providers—one in which people take a more active role in their own care decisions.
PCC moves beyond the traditional disease-focused model to place a greater emphasis on patients’ unique needs, preferences and values. It also prioritizes safety, which, according to one member of the Sermo community, “is the foundation of good patient care. Achieving safety in patient care is part of achieving quality patient care.”
Here’s how it improves patient care standards, plus 13 actionable ways healthcare organizations and doctors can apply PCC in practice.
Why is patient-centric care so important?

The U.S. healthcare system aims to deliver evidence-based, high-quality and cost-effective care that optimizes patient outcomes. To achieve this, it has increasingly relied on evidence-based medicine (EBM)—or evidence-based practice (EBP)—and PCC conjunctively.
While EBM’s standardized protocols can conflict with the individualization PCC requires, medical centers that effectively integrate both approaches support patients more holistically, improving outcomes and reducing the risk of error.
Here are some more reasons to explore PCC:
More comprehensive support
A common misconception is that PCC simply means granting all patient requests. But it involves:
- Identifying and responding to patients’ perspectives and emotional needs
- Working together to establish a mutual understanding of the condition, its treatment, and the roles of both physician and patient
These two points reflect PCC’s core principle: Healing depends not only on accurate diagnoses, but also on understanding and treating each patient as a whole person.
Stronger patient satisfaction
Individualized care improves patient satisfaction in several ways. Research shows that patients who receive PCC are more than four times likelier to report improved physical health, and over five times likelier to report improved mental health. PCC also enhances patients’ sense of treatment necessity more than sixfold.
Patient satisfaction also reduces costs, prevents discharge/readmission cycles and strengthens patient-clinician communication.
Lower the risk of error
When physicians combine components of PCC, like patient education, standardized policies and co-creation of care plans, they empower both themselves and their patients to understand situations and spot problems before they snowball. This error reduction improves patient outcomes and quickens care processes.
The 4Cs of quality patient care

The four core primary care functions—often called the four pillars, tenets or the 4Cs—were first developed in the 1990s to improve service quality. Since then, they’ve informed PCC’s frameworks and helped physicians measure and advance their quality of care.
The 4Cs are first contact, comprehensiveness, coordination and continuity:
Contact
“Contact,” or “first contact,” refers to the initial point that patients enter the healthcare system through a primary care provider. Its function is to help patients seek care for new health concerns and give them timely, individualized treatment when needed.
Comprehensiveness
“Comprehensiveness” refers to the scope of services available to address a wide range of patient needs, including preventive, curative, rehabilitative and palliative services. Its function is to ensure that providers can manage most common conditions and collaborate with necessary specialists.
Coordination
“Coordination” refers to how primary care integrates services within and beyond the practice setting. It encourages key stakeholders to communicate effectively, giving patients a seamless transition across various levels and types of care.
Continuity
“Continuity” refers to the ongoing, long-term relationship between patients and their primary care providers. Through routine interactions across time, providers should build a holistic understanding of patients’ health histories, preferences and needs—a process that improves patient care.
How to improve quality of care in healthcare: 13 actionable PCC strategies
While several PCC frameworks exist, very few offer clear, actionable guidance for translating principles into everyday clinical practice.
To help address this problem, researchers from the University of Calgary’s Cumming School of Medicine and Department of Economics developed a conceptual framework guided by the Donabedian model: structure, process and outcome.
Here are 13 ways to improve patient care and put PCC into practice, each drawn from the framework above—seven at the structural level, four at the process level and two at the outcome level.
Structure
Strategies under “structure” relate to system‐ and organizational‐level stakeholders—such as senior leadership and policymakers—who establish the foundational supports necessary for patient‐centered care.

1. Incorporate a PCC culture
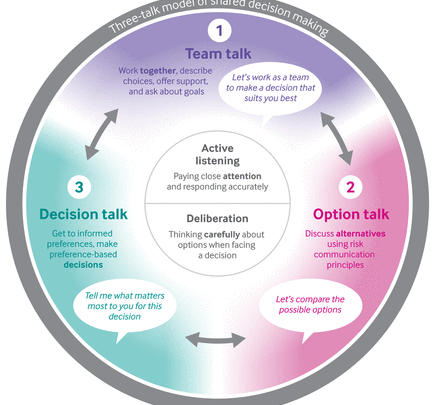
Leaders should implement an organization-wide, unified vision that emphasizes respect for diverse patient values and lived experiences. This can include standardizing PCC terminology, recognizing the role of diversity in holistic care and ensuring that shared decision‐making guides policy decisions.
2. Co-design training programs
Collaborate on training program development and implementation to standardize PCC training organization-wide. These programs should:
- Integrate both patient and provider perspectives
- Extend beyond formal curricula to include mentorship and ongoing leadership development
- Involve all stakeholders—including administrative staff and volunteers—to ensure a sustained cultural shift toward PCC in day-to-day practice
3. Collaborate on health promotion and prevention
Policymakers, leaders and local organizations should co-design health promotion and prevention efforts to match the lived experiences of their patient populations. The more perspectives available, the more information goes into these efforts, leading to comprehensive plans.
4. Commit your workforce to PCC
Provide clinicians with the resources and incentives they need to practice person-centered care. This can involve:
- Adopting payment models that favor relationship‐building
- Internally celebrating small wins related to PCC
- Creating “communities of care,” which foster teamwork among key stakeholders to collectively meet patients’ needs
5. Provide an accommodating environment
A healthcare environment’s physical design—for example, natural lighting and noise control—influences both patient safety and perceived experiences. Beyond creating an environment that prioritizes safety, partner with patients to create settings that are welcoming, private and accommodating of individual needs.
6. Support the relevant technological infrastructure
Implement the necessary infrastructure for electronic health records and patient portals that connect providers throughout the care continuum. Systems should be both seamless and user-friendly. And all relevant professionals should receive training and ongoing technical support to make sure they (and their patients) can securely access and use these systems.
7. Measure PCC
With input from patients, co‐design frameworks and meaningful metrics for measuring, monitoring and evaluating PCC—accounting for both complaints and compliments. Use these frameworks to identify gaps and drive improvement.
Process
The strategies under “process” involve front‐line and service‐delivery stakeholders.
8. Cultivate communication
There are two sides to the communications coin: listening and responding. As you listen to patients, aim to take an active role. Ask questions out of genuine concern, respond empathetically and consider your nonverbal behaviors. As you respond and share information with patients, work to create a shared understanding and tell patients all relevant details.
One Sermo community member shared valuable insight about the importance of patient care about advances in medical technology. They wrote, “The physician plays a fundamental role at the intersection between medicine and technology, acting as the bridge between technological innovations and [PCC].”
“To maximize the benefits of these technologies, it is essential that we as health professionals act as guides and advocates, ensuring that patient-centered care remains the priority.”

9. Provide compassionate care
Respectful and compassionate care means being responsive to individual patient needs. Recognize the patient as an expert on their own health, and take the time necessary to understand the patient’s psychosocial context. In all cases, aim to build a partnership with patients—one built on empathy and transparency.
10. Engage patients in care management
Co-designing care plans gives patients an active role in managing their condition. This involves promoting health literacy, facilitating shared decision-making and actively gathering patient feedback, all of which can lead to better outcomes.
11. Ensure integrated care
Use unified digital platforms to securely and seamlessly communicate information to all key stakeholders across the continuum, and actively address any communications process fragmentations. For maximum transparency and ease of access, give patients a private and direct line to their digital records.
Outcome
“Outcome” strategies involve the ways patients, families and medical practices measure and further utilize existing PCC initiatives.
12. Measure access to care
Evaluate your system’s capacity to promptly and effectively deliver PCC. This involves systematically measuring the time it takes for patients to receive care, the impact of financial barriers and physician availability.
13. Consider patient self-reporting
Patient‐reported outcomes measures (PROMs), patient‐reported experience measures (PREMs) and patient‐reported adverse outcomes (PRAOs) all capture critical patient‐generated information. Together, they offer direct insight into key focus areas like patients’ daily functioning and care experiences.
Providers who integrate patient input into clinical practice improve outcomes and deliver higher-quality care. Use these metrics to inform future PCC initiatives.
Join a global network of physicians to improve care together
Other physicians’ input can give you tips and insights you wouldn’t find otherwise. See what other professionals have to say by joining the exclusive Sermo community of verified physicians.
Sermo is home to a community of 1.5 million physicians and other HCPs who collaborate with their peer groups, share insights and learn together. Plus, Sermo offers doctors the opportunity to earn a healthy side income through paid surveys that help improve healthcare.
Become a Sermo member today and join a global network of doctors.