April is STD Awareness Month. Over the month, the CDC has been presenting a series of posts around this year’s theme, “Syphilis Strikes Back” to help inform you about real-life implications for your practice and your patients. You’ll hear it here first on Sermo! Last week, Dr Gail Bolan discussed the complexities of syphilis in the US. Today, in her final installment of this series, Dr Bolan tests your knowledge with two syphilis case studies.
Sermo: Test Your Knowledge with Two Syphilis Case Studies
By: Dr. Gail Bolan
In our final week, I want to share two case studies with you to illustrate just how challenging it can be to put working knowledge about syphilis into practice.
Hint: There are five missed clinical and public health opportunities between these two cases. See if you can spot them all.
Missed Opportunity Case #1
- June 5 – A 40-year-old man living with HIV sees his provider because of a rash on his buttocks. His provider believes it is folliculitis.
- June 26 (3 weeks later) – He returns to his provider with a rash over his entire body and scalp, including the unresolved rash on his buttocks. His provider now believes the rash to be herpes zoster and treats with valacyclovir.
- July 3 (1 week later) – He returns to his provider once again because the rash is not healing. Having done independent web-based research (i.e., a Google diagnosis), the patient requests serologic testing for syphilis. A quantitative nontreponemal test (in this case, an RPR) and confirmatory treponemal test are ordered.
- July 5 – Provider receives the lab results of an RPR titer of 1:128 and a reactive treponemal test. Based on lab results and physical exam, patient is diagnosed with secondary syphilis.
- July 11 (more than 5 weeks after the initial visit) – Patient returns for treatment and is treated with benzathinepenicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1-week intervals.
Missed Opportunity Case #2
- September 2 – 34 year-old theology student presents to the student health center with reddish, crusted lesions on his penis. He is treated with fungal cream.
- September 9 (1 week later) – He returns because the lesions are not getting better and he is prescribed dicloxacillin for a presumed staph infection.
- December 21 (over 3 months after the initial visit) – The lesions on his penis have resolved and he now returns with a rash on his trunk and sees a different provider who knows the patient is a man who has sex with men. Suspecting secondary syphilis, this provider orders an RPR and treponemal test. The patient is then treated empirically for secondary syphilis with benzathine penicillin G 2.4 million units IM in a single dose. The provider reports the case of secondary syphilis to the health department.
*** Warning! Spoilers Below***
What went wrong? In both cases, the following missed opportunities in clinical and public health management occurred:
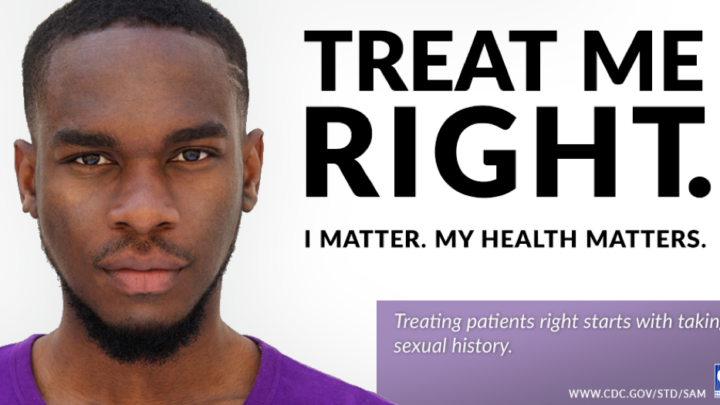
- Sexual history taking was absent. A sexual history would have allowed the provider to identify each patient’s syphilis risk factors, appropriate tests to order and if treatment for presumptive infectious syphilis should be given at the initial visit.
- Symptoms of infectious syphilis were misdiagnosed. In case #1, the patient’s secondary syphilis rash was thought to be folliculitis or herpes zoster. In case #2, the patient’s primary syphilis chancres were thought to be a fungal or staph infection. Both patients left the clinic with untreated infectious syphilis and without syphilis in the differential diagnosis.
- Empiric treatment was not provided during the initial symptomatic visit. If a sexual history would have been taken, the provider in each case would have learned that his/her patient’s symptoms could be due to infectious syphilis because both patients where at high risk for syphilis. The delay in time to treatment put the patient at risk of progressing to more serious syphilis complications, such as ocular syphilis and neurosyphilis. It also presented a public health threat since a patient with untreated infectious syphilis can potentially transmit the disease to additional sex partners and is more likely to acquire or transmit HIV to their sex partners. Any patient at risk for syphilis with signs or symptoms suggestive of primary or secondary infection, or a patient who reports they are a contact to a case of syphilis, should be treated presumptively for early syphilis at the initial visit without waiting for syphilis test results.
- The healthcare provider or laboratory did not report the syphilis case or positive syphilis test results to the health department. Both healthcare providers and laboratories are required by law to immediately report suspected cases of syphilis by stage and positive syphilis laboratory test results, respectively, to their local or state health department.
Additionally, there was a fifth missed opportunity in case #1:
- 5. RPR was not ordered on the day of treatment. Serologic response to treatment is assessed by comparing follow-up nontreponemal test titers to the titer obtained right before treatment. Titers change as the natural history of syphilis progresses and in the early stages can increase significantly, while the patient is returning for treatment.
And for all of you overachievers out there, here’s a bonus round:
In case #1, the patient was over-treated! Patients living with HIV who have primary or secondary syphilis should be treated as those without HIV infection. In this case, the patient only needed to receive one dose of benzathine penicillin G.
Resources:
-
- Evaluating Patients for Primary Syphilis: http://californiaptc.com/wp-content/uploads/2016/10/primary_syphilis_printable-2011.pdf (note that the STD Treatment Guidelines in this document have been updated since this was developed; the most recent guidelines are included in the final bullet)
- Evaluating Patients for Secondary Syphilis: http://californiaptc.com/wp-content/uploads/2016/10/secondary_syphilis_printable_2011.pdf (note that the STD Treatment Guidelines in this document have been updated since this was developed; the most recent guidelines are included in the next bullet)
- CDC’s 2015 STD Treatment Guidelines:
This is the final blog entry in a series on syphilis prevention that we’ve been doing throughout the month. I hope these posts not only inform but prompt discussion about the syphilis challenges and opportunities that you face in your work.
Sermo wants to know: How many missed opportunities were you able to spot? Has this syphilis blog series been helpful to you? Login or join Sermo to join the conversation.