April is STD Awareness Month. Over the month, the CDC will be presenting a series of posts around this year’s theme, “Syphilis Strikes Back” to help inform you about real-life implications for your practice and your patients. You’ll hear it here first on Sermo! Last week, Dr Gail Bolan discussed the rise of congenital syphilis in the US and the dangers of syphilis infection during pregnancy. Today, Dr Bolan goes over the complexities of syphilis.
Understanding the Complexities of Syphilis
By Dr. Gail Bolan
When I was a medical student at Dartmouth in the mid-‘70s, a professor told me in no uncertain terms that I would never see a case of syphilis. Flash forward to 1987, I’m now the STD Prevention and Control Director in the San Francisco Department of Public Health, and not only are we seeing syphilis, we would soon be fighting a substantial outbreak. The fight against syphilis continues to this day – and not just in San Francisco but across the nation. Although it sometimes feels discouraging to still be facing down this ancient disease, I’m hopeful that you can draw from my experience in your own practice.
Today, 1 in 3 surveyed physicians haven’t received post-medical school training in STDs. And if knowing syphilis is knowing medicine, then what we now have are too many providers who find themselves at a great disadvantage. Be honest with yourself, is syphilis even on your radar? I’m guessing many of you have had limited, if any, experience with diagnosing and treating it. So let’s start with the basics:
- Know the variety of signs and symptoms – it’s a downright necessity. There’s a reason we call syphilis ‘the great imitator,’ so be mindful that not every patient will have a classic presentation of the disease. For instance, primary syphilis does not always equal a solitary chancre. It is not uncommon for patients to present with multiple lesions. So, the differential diagnosis for a patient presenting with genital lesions should include primary syphilis. In the same vein, secondary syphilis will not always present with a classic palmar/plantar rash.
- Talk with your patients, it’s a must. Routinely take a sexual history to identify who is at risk and who needs testing.
- In addition to a sexual history, provide a thorough physical exam. Many patients do not notice the signs and symptoms of syphilis. These can include chancres hidden in the vagina, rectum, or mouth; easy-to-miss faint macular rashes; nonspecific flu-like symptoms; and condyloma lata masquerading as genital warts. It will be up to you to spot them.
- Stage the patient’s syphilis case appropriately – it is a difficult but critical step to determine the treatment that a patient should receive. Accurate staging takes into account the information obtained through a sexual and medical history, physical exam findings, and nontreponemal and treponemal test results. In addition, work with the health department – they may be able to provide other vital details which include prior syphilis test results, treatment history, and sexual contacts.
Understanding these individual clinical pieces can help you to identify and diagnose cases of syphilis in a timely manner.
And though syphilis has been around a long time, it somehow manages to keep us on our toes. Enter ocular syphilis – a clinical manifestation that can occur at any stage of the disease. With an increased number of these cases being reported among patients with syphilis, there are several things you should keep in mind:
- Assess all patients with syphilis for neurologic abnormalities, including visual complaints such as vision loss, blurry vision, eye pain, and/or eye redness.
- Test patients at high risk for syphilis and presenting with neurologic or ocular symptoms for syphilis and HIV.
Now that you’ve had a brief refresher on syphilis basics and a quick overview of ocular syphilis, we’ll spend our final week digging into a few real-life case studies.
Resources:
- A Guide to Taking a Sexual History: https://www.cdc.gov/std/treatment/sexualhistory.pdf
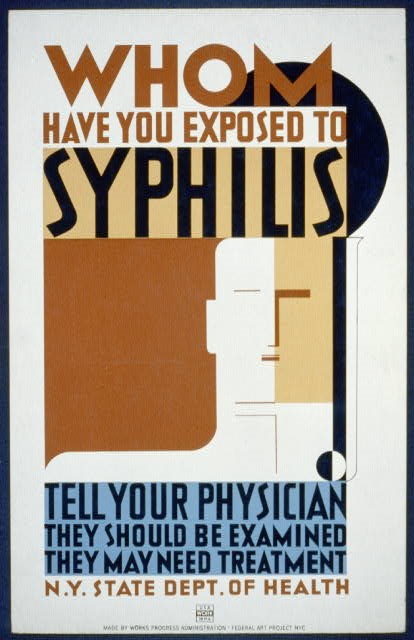
- Detailed syphilis fact sheet: Syphilis images:
- STD Treatment Guidelines (Syphilis):
- Clinical Advisory:
- Syphilis Self-Study Module: http://www.std.uw.edu/go/pathogen-based/syphilis/core-concept/all
This is the third blog entry in a series on syphilis prevention that we will be doing throughout the month. I hope these posts not only inform but prompt discussion about the syphilis challenges and opportunities that you face in your work.
Sermo wants to know: How do you start your sexual history conversations with patients? Login or join Sermo to join the conversation.