By Dr. Donna Sweet
There is no doubt in my mind that the HIV epidemic is continuing in the United States. With so much progress being made around HIV prevention and treatment, you wouldn’t think I would be seeing patients who have an AIDS diagnosis the first time they are seen as an HIV positive patient. But I saw two of them within a week of each other earlier this year.
One of them, a 33-year-old MSM had seen multiple providers complaining of weight loss and fatigue before presenting to the hospital with sepsis and pancytopenia. His HIV test was positive with a CD4 cell count of 3 and blood cultures positive for histoplasmosis—an advanced AIDS diagnosis. Routine HIV testing and diagnosis would have helped this patient get linked to care more quickly and avoid an AIDS diagnosis.
But HIV is still something that many physicians feel they don’t need to think about or test for. On National HIV/AIDS Testing Day and every day, it’s important for healthcare providers to remember that all patients 15-64 need to be tested at least once in their lives and more often if their behavior puts them at higher risk for HIV infection. It’s true that most patients will be negative. But, if you haven’t already discussed your patient’s sexual activity, a negative HIV test result is a good way to open the conversation and take the next step to keep your patients healthy and free of HIV.
When I take a sexual history, I use the 5P’s of sexual health. These include: Partners—the number and gender of partners over time, Practices—types of sexual practices, Protection from STIs, Past history of STIs, and Prevention of Pregnancy. If this conversation reveals signs of substantial HIV risk, as shown in this table, then it’s time to take the next step and talk about PrEP—HIV pre-exposure prophylaxis.
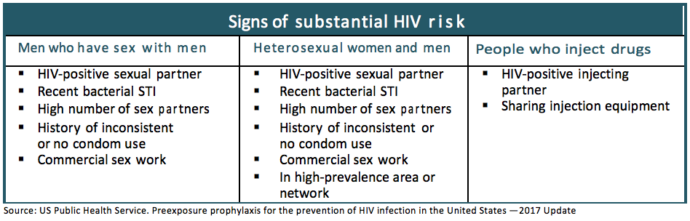
PrEP is 90-92% effective in preventing HIV infection. So, when I talk to a patient with substantial risk—often an MSM in his early 20s, who finds that he has an HIV-positive partner, or is concerned about a condom breaking or doesn’t use them—I let him know that PrEP can offer important protection against HIV infection.
Before starting a patient on PrEP it’s critical that you do an HIV 4th generation assay and test for other STIs such as syphilis, gonorrhea, and chlamydia. Be sure to test the site of sex or an STI may be missed. Also check Hepatitis B status. Truvada (tenofovir disoproxil fumarate and emtricitabine) is the only medication currently approved for PrEP. It is not indicated or appropriate for Hepatitis B—but it treats it. And someone taking PrEP may have a flare-up of Hepatitis B if PrEP is stopped.
There are new PrEP resources available. The recently published 2017 PrEP Guidelines are now available from the Centers for Disease Control and Prevention (CDC). The CDC Act Against AIDS program also has Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP) websites with Resources for Providers to with prescribing both HIV PrEP and PEP. These are great resources to help us take the next steps to fight the HIV epidemic and ensure our patients lead healthy lives.