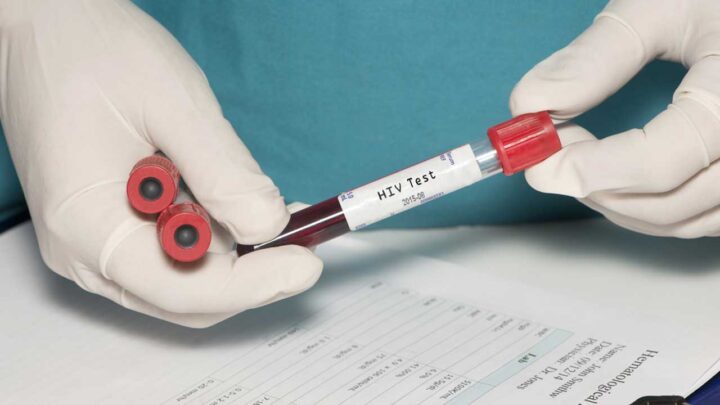
The Centers for Disease Control and Prevention (CDC) recommends universal screening to ensure every patient is tested for HIV as a part of standard care. According to CDC, people between the ages of 13 and 64 should be tested for HIV at least once as part of routine health care and those with ongoing risk factors should be screened at least annually.
Since risk-based HIV screening can result in missed opportunities to link patients to the HIV prevention and treatment services they need, universal screening is the standard of care.
Here are 5 key reasons why health care providers should adopt universal screening:
- Universal screening ensures equitable care for all patients. HIV crosses the boundaries of gender, sexual orientation, age, race, and ethnicity. HIV screening should, too.
- It can reduce HIV stigma. Making HIV screening a routine health care practice, like checking blood pressure, helps to normalize screening and reduce HIV stigma for patients and other clinicians.
- Universal screening is an opportunity to talk to your patients about other ways to prevent HIV, such as (or including) pre-exposure prophylaxis (PrEP). PrEP is a powerful tool to prevent getting HIV through sex or injection drug use. Any licensed prescriber can prescribe PrEP.
- It helps to improve patient outcomes. In 2021, more than 1 in 5 people who received an HIV diagnosis already had the most advanced stage of the disease. With earlier diagnosis, people can get the HIV treatment and care they need sooner, and they can have longer, healthier lives.
- Universal screening will help to end the HIV epidemic. About 40% of new HIV infections can be attributed to people whose HIV is undiagnosed and who are unaware they have HIV. Diagnosing HIV quickly and linking people to treatment immediately are crucial to reducing new HIV infections.
Here are some potential challenges you, your peers, and your patients may face with universal screening in your practice, and how you can address them.
For Clinicians
If you or your colleagues are hesitant to use universal screening, keep in mind that:
- Although some clinicians may believe that only certain types of people are at risk for HIV, anyone can get HIV and everyone should be tested.
- Clinicians should treat HIV nonjudgmentally, like they would other chronic conditions such as high cholesterol. HIV screening should be the standard of care for everyone.
- Sexual health is an essential element of overall health and well-being. While it may be a little uncomfortable to have these conversations, you can help normalize them by routinely discussing sexual health with your patients. View CDC’s conversation starters and resources on how to take a sexual history.
For Patients
If some patients do not think an HIV test is right for them, you can:
- Make it clear you screen all your patients for HIV.
- Reassure your patients that HIV screening is a part of routine health care, like monitoring their vital signs.
If patients are hesitant to take an HIV test in clinic, consider offering the option of an HIV self-test :
- Self-testing makes testing more convenient and accessible for all; it can be performed when and where the patient feels most comfortable and in a private setting, like their home.
- Sharing the option of HIV self-testing with your patients can help normalize HIV screening and reduce stigma.
- Your patients can order up to two FREE self-tests every 90 days through Together Take Me Home.
Want to learn more about how to incorporate universal HIV screening in your practice? You can download CDC’s Integrating Routine HIV Screening in Your Practice brochure from HIV Nexus.