April is STD Awareness Month. Over the month, the CDC will be presenting a series of posts around this year’s theme, “Syphilis Strikes Back” to help inform you about real-life implications for your practice and your patients. You’ll hear it here first on Sermo! Last week, Dr. Gail Bolan set the stage with an overview of Syphilis in the United States. Today, Dr. Bolan discusses the rise of congenital syphilis in the US and the dangers of syphilis infection during pregnancy.
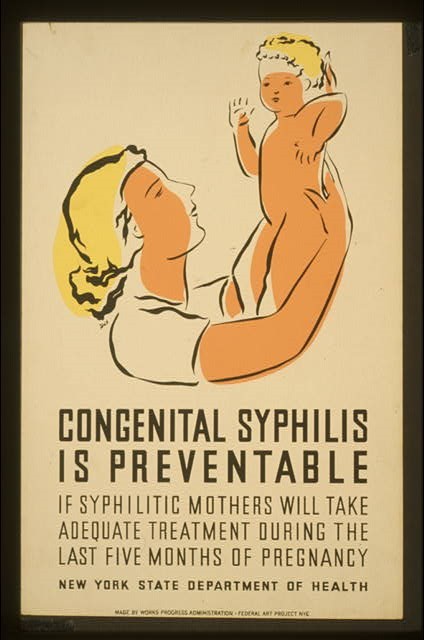
Congenital Syphilis Surges in the U.S.
By Dr. Gail Bolan
Would you be surprised to learn that congenital syphilis (CS) is on the rise? Don’t be. Increases in syphilis among women in recent years have led to the highest number of CS cases since 2001. Even a single case is considered a failure on the part of public health and healthcare systems, so you can understand our concern with the nearly 500 cases in 2015. Preliminary data suggest these numbers will continue to climb.
The dangers of syphilis infection during pregnancy – and the significant health problems for an infant – should not be understated. Historical data indicate that up to 40% of pregnancies in women with untreated syphilis will result in miscarriage, stillbirth, or infant death. Infants who live may develop severe illness, including skeletal abnormalities; hepatosplenomegaly; jaundice; anemia; optic atrophy; interstitial keratitis; sensorineural deafness; or meningitis, which can cause developmental delays and seizures. And yet, congenital syphilis is preventable.
We are calling on clinicians to get back to the basics of syphilis prevention for pregnant women. There isn’t a new strategy to reverse this growing problem. We just need everyone to do what we know works—what has always worked. Here are actions you can take:
- Screen all pregnant women for syphilis at their first prenatal visit.
- Women at high risk should be rescreened early in their third trimester and again at delivery. This includes women with a history of sexually transmitted infection, incarceration, drug use, [or] multiple or concurrent partners, and those who live in areas with high rates of syphilis.
- Take immediate action if your patient is diagnosed with syphilis. Pregnant women diagnosed with syphilis should be treated with long-acting benzathine penicillin G IM immediately. Treatment at least 30 days prior to delivery is likely to prevent congenital syphilis.
Refer your patients elsewhere if the correct treatment is not available onsite. Follow-up with your patient and document the treatment received. If a pregnant patient is lost to follow up before treatment could be documented, contact your local health department’s STD program for assistance.
- All cases of syphilis and congenital syphilis should be reported to your state or local health department right away. CDC recommends reporting within 24 hours and also indicating pregnancy status.
- Advise your patient to tell her sex partner or partners about the infection and encourage them to get tested and treated to avoid reinfection.
- Before discharging any mother or newborn infant from the hospital, make sure that the mother’s serologic syphilis status was documented at least once during her pregnancy. If the test is positive, ensure that the mother and baby are evaluated appropriately before discharge and, if necessary, treated. Also, if a woman delivers a stillborn infant, she should be tested for syphilis.
- Keep in mind that the same tenets of quality sexually transmitted disease prevention apply to pregnant women, too. Take a sexual history throughout the course of your patient’s pregnancy, and talk with her about prevention methods.
Resources:
- CDC STD Treatment Guidelines – Syphilis During Pregnancy: https://www.cdc.gov/std/treatment-guidelines/syphilis-pregnancy.htm
- Screening recommendations: https://www.cdc.gov/std/treatment-guidelines/screening-recommendations.htm
- STDs during Pregnancy Fact Sheet: https://www.cdc.gov/std/treatment-guidelines/pregnant.htm
- AtlasPlus (to explore CDC’s HIV, Hepatitis, STD, and TB data):
This is the second blog entry in a series on syphilis prevention that we will be doing throughout the month. I hope these posts not only inform but prompt discussion about the syphilis challenges and opportunities that you face in your work.
Sermo wants to hear from you: Are you screening all pregnant patients at their first prenatal visit? Are you doing any additional syphilis screening on these patients? Login or join Sermo to join the conversation.