
The Centers for Disease Control and Prevention (CDC)
On June 5, 1981, the first five cases of what would later become known as HIV were officially reported in the Centers for Disease Control and Prevention’s (CDC’s) Morbidity and Mortality Weekly Report (MMWR). Forty years later, we have seen tremendous scientific and medical advancements in the treatment and prevention of HIV and AIDS that have led to a 73% decrease in HIV incidence from the height of the HIV epidemic in 1984/1985 to 2019.
Despite this extraordinary progress, we still have work to do. The United States sees approximately 35,000 new HIV infections per year, and some racial and ethnic communities continue to be disproportionately affected by HIV. According to data from 2019:
- Black or African American people account for 42% of new HIV infections, yet represent only 13% of the U.S. population; and
- Hispanic or Latino people account for 22% of new HIV infections while making up only 19% of the U.S. population.
At the front lines of the HIV epidemic, health care providers have a unique opportunity to address racial and ethnic HIV disparities by ensuring equitable access to HIV testing and treatment services and prevention strategies for those disproportionately affected by HIV. Below we discuss three ways providers can help end the HIV epidemic for patients of all races and ethnicities.
1. Implement Routine HIV Screening
Early diagnosis of HIV is critical for reducing HIV incidence and improving health outcomes for people living with HIV. Yet, 13% of people with HIV in the United States are unaware of their HIV status, and knowledge of HIV status is lower among racial and ethnic minority groups than among White people. Providers can promote health equity in their practices by making routine HIV screening the standard of care. Moreover, by offering HIV screening to every patient, providers can remove the stigma around HIV and empower all patients to know their status. CDC’s Screen for HIV Toolkit has practical tips for routine HIV screening.
2. Prescribe PrEP to Prevent HIV
Pre-exposure prophylaxis (PrEP) is a powerful tool for preventing the acquisition of HIV. Studies show that when taken as prescribed, PrEP is about 99% effective in preventing HIV from sex and at least 74% effective in preventing HIV from injection drug use. CDC recommends that health care providers prescribe PrEP to any patient who is at risk for acquiring HIV from sex or injection drug use. However, only 23% of individuals who could benefit from PrEP were using it in 2019. That same year, PrEP coverage was more than 50% higher among White people at risk for HIV than among people of other races or ethnicities.
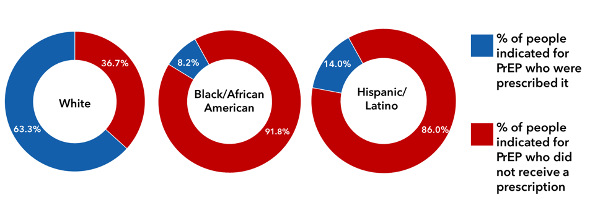
*Data represented only available for white, Black/African American, and Hispanic/Latino populations
CDC offers a <PrEP and PEP for HIV Prevention Toolkit to answer providers’ most frequently asked questions about how to prescribe HIV prevention.
3. Address Patient Barriers to HIV Treatment
HIV medicine, called antiretroviral therapy (ART), is recommended for all people with HIV. When taken as prescribed, ART can help people with HIV suppress their viral load, maintain high CD4 counts, prevent the more advanced stages of HIV, and live long and healthy lives. However, patients may experience barriers that prevent them from adhering to their treatment plan, such as treatment costs, lack of stable housing and transportation, and fear of disclosing their HIV status. CDC’s <HIV Care Is Prevention Toolkit includes materials to help providers identify common barriers that patients may experience so that they can work together with patients to address their needs.
Here is more of what Sermo physicians have to say about advancing health equity to end the HIV epidemic:
Only 40 years since the first cases of AIDS were reported in the US, we have the tools to ensure no one gets sick. We can end stigma and we can end HIV.
Dr. Demetre Daskalakis, MD, MPH
As clinicians, we have a responsibility to meaningfully address racialized health inequities through patient-centered HIV care.
Dr. Oni Blackstock, MD, MHS
Achieving health equity in HIV care starts with screening every patient for HIV, facilitating conversations about prevention options like PrEP, and helping patients overcome barriers to care.
Dr. David Malebranche, MD, MP
Physician Assistants are vital practitioners and advocates of HIV prevention, testing, and treatment. We are ready to play our part in ending the HIV epidemic.
Diane Bruessow, MPAS, PA-C, DFAAPA
Everyday thousands of Sermo member physicians from diverse backgrounds and experiences exchange knowledge with each other. Sermo is the original medical social network that empowers today’s physicians. Over 1 million fully verified physicians across more than 150 countries come to our platform to talk with peers, participate in paid medical studies, solve challenging patient cases, contribute to the world’s largest database of drug ratings – and enjoy a few laughs along the way.
Interested in more? Check back any time and follow us on Facebook, Twitter, and LinkedIn for the latest and greatest in physician insights.