For reasons that are unclear to me, ICD-10 was foisted on physicians in 2015 and mandated by CMS.
Now, when classifying heart failure one is consistently badgered by hospital coding monitors to specify whether a patient has systolic heart failure, diastolic heart failure (I50.3- (Diastolic (congestive) heart failure)) or combined systolic and diastolic heart failure.
The preferred term for diastolic heart failure is now heart failure with preserved EF (HFpEF) or huff puff because most of these patients don’t have anything that clearly documents “diastolic dysfunction and it has become clear in recent years that many of these patients are limited, not by cardiac dysfunction but by key nondiastolic features such as limited systolic reserve, abnormal volume regulation, and maladaptive ventricular–arterial interaction
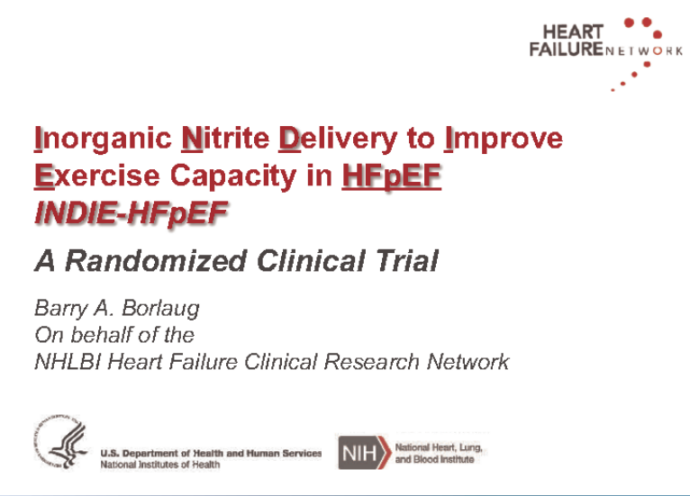
A recent trial of inhaled inorganic nitrites presented at the American College of Cardiology meeting recently in Orlando further emphasizes a) how complicated the diagnosis of HFpEF is and b) how ineffective all drugs are for treating it.
The INDIE investigators hypothesized that inorganic nitrite, which restores nitric oxide, would improve exercise capacity and clinical status in patients with HFpEF given evidence suggesting that impaired nitric oxide signaling plays a role in heart failure.
For the INDIE-HFpEF trial, researchers across 20 centers participating in the NHLBI Heart Failure Clinical Research Network randomized 105 patients to inhaled nitrite versus placebo in a cross-over trial.
The results were disappointing as the drug had no effect on peak exercise capacity measured by cardiopulmonary exercise testing and did not increase daily activity or patient-reported quality of life nor decrease cardiac congestion.
I pulled up the complete inclusion criteria for this trial (https://clinicaltrials.gov/ct2/show/NCT02742129) and the 12 inclusion and 21 exclusion criteria give us an idea of how complicated the HFpEF diagnosis is.
It’s interesting that inclusion criteria #4 contains the only mention of Echo/Doppler criteria.
To be considered HFpEF patients had to have
One of the following :
◦Previous hospitalization for HF with radiographic evidence (pulmonary venous hypertension, vascular congestion, interstitial edema, pleural effusion) of pulmonary congestion or
◦Catheterization documented elevated filling pressures at rest (PCWP ≥15 or LVEDP ≥18) or with exercise (PCWP ≥25) or
◦Elevated NT-proBNP (>400 pg/ml) or BNP(>200 pg/ml) or
◦Echo evidence of diastolic dysfunction/elevated filling pressures manifest by medial E/e’ ratio≥15 and/or left atrial enlargement and chronic treatment with a loop diuretic for signs or symptoms of heart failure
An actual measurement of diastolic function of the myocardium (say tau for relaxation or stiffness constant for compliance) is clearly not required for the diagnosis of HFpEF and is not really measurable by noninvasive parameters.
The echo parameter of E/e’ > 15 is primarily a measure of preload (and it is fairly inaccurate in patients with normal EF)
What are the take-home points from this trial:
- Another potential drug treatment for HFpEF has failed, joining the dozens already which don’t help.
- HFpEF is not synonymous with myocardial diastolic dysfunction
- Echo/Doppler diastolic parameters are primarily useful for vaguely estimating LV preload and play only a limited role in diagnostic criteria for HFpEF.
Read Dr. Pearson’s previous posts from this year’s ACC:
- ACC18: Pricey Praluent Proves Beneficial (sort of) Post ACS
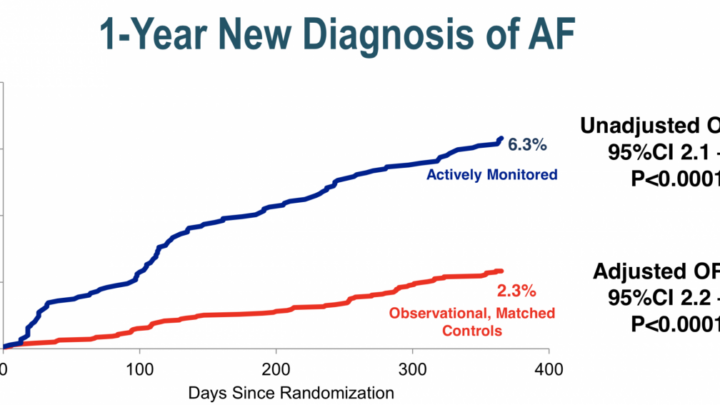
- ACC.18: Subclinical Afib: Seek (with Zio) And Ye Shall Find
Login or join Sermo to contribute your opinions to this post.
Dr. Anthony Pearson is a clinical cardiologist and director of noninvasive cardiac imaging at St. Luke’s Hospital in St. Louis, Missouri. In his spare time he plays keyboards and guitar in the band, Dr. P and the Atherosclerotics. Blog: www.theskepticalcardiologist.com | Twitter: @skepcard