As States Ease Up on Restrictions, Accurate Testing and Tracing are Critical to Stopping Disease Spread and Virus Reinfection
NEW YORK— May 14, 2020 —The United States has performed over 9.9 million molecular tests for COVID-19 to date. The ability to accurately test and trace new infections is critical for reopening the country. Experts believe easing restrictions before testing becomes more accurate and accessible could lead to a new surge of infections.
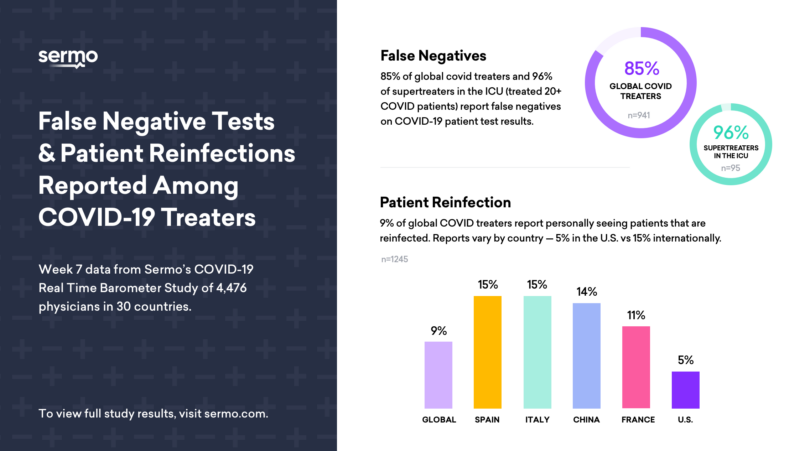
Sermo’s COVID-19 Real Time Barometer, an international weekly poll including more than 40,000 interviews with physicians in 31 countries, explores a variety of COVID-19 themes. In week 7, perspectives around false negatives and re-infection rates were explored. The survey included 4,476 physicians and was conducted May 3 – 5, 2020. Complete study data and methodology can be found here.
False Negatives
- 85% of physicians surveyed state they have seen some degree of false negative test results.
- 96% of “Supertreaters” in an ICU setting – highly experienced physicians who have treated over 20 COVID-19 patients – believe they have seen COVID-19 tests produce a false negative.
- 37% of physicians in the hospital consider more than 20% of the tests have produced false negatives.
False Positives
- Conversely, 41% of physicians reported seeing at least one false positive where someone who does not have the virus tests positive.
These inaccuracies present challenges to understanding the pandemic, controlling the spread of the disease, preventing re-infections and ultimately reopening economies.
It has been hypothesized the reasons COVID-19 tests may be unreliable and often present false negatives are inadequate or faulty sample collection (swabbing technique), timing of sample collection, test sensitivity, test design and shortages of reagents needed to start up and run the tests. Any one of these can create a false negative test.
Test manufacturers as well as leading health organizations, including the U.S. Food and Drug Administration and the U.S. Centers for Disease Control and Prevention, have not confirmed how common false negatives are. While the FDA requires manufacturers to report any known instances of false negatives as a condition of granting provisional approval, no such reports are available from the agency.
Re-Infection Phenomenon
According to the World Health Organization, “There is currently no evidence that people who have recovered from COVID-19 and have antibodies are protected from a second infection;” however, some experts feel immunity to the virus is not yet fully understood.
As immune response is investigated, physicians on the frontlines are seeing patients being re-infected shortly after they recover from COVID-19.
- In fact, 9% of worldwide physicians polled by Sermo believe they have seen a patient with a re-infection.
- Perceived re-infection rates vary widely among countries; only 5% of U.S. doctors report seeing re-infection versus 15% internationally.
- For example, in Italy and Spain, 15% of physicians have encountered re-infected patients, and in China, 14% of those surveyed saw re-infections.
The cause(s) of reinfection are unclear, but may be due to:
- Inaccurate tests: initially, a patient might have received a false negative or when re-infected, might have experienced a false positive;
- Reactivation of the virus or a patient had not fully recovered from the disease;
- Patient engaged in new or repeated contact with an infected person.
Respondents in Sermo’s Barometer shared:
“We saw a patient who was treated with remdesevir and tocilizumab. He was resolved and then somehow re-infected. We did not find the cause of the re-infection.”
“Either the patients are re-infected or the follow-up tests were false negative followed by true positive.”
“I treated a young patient with mild COVID-19 and PCR (polymerase chain reaction) symptoms who was admitted to the hospital and then released. This individual returned five weeks later with severe unilateral PCR and pneumonia.”
These cases demonstrate an uncertainty of disease persistence or actual re-infection.
As tests are improved and more accessible, physicians will begin to feel confident screening patients prior to medical procedures and surgeries that have been postponed during the height of the coronavirus pandemic. Physicians feel the following patients should require COVID-19 pre-screening before an office visit or procedure:
- 78% said transplant patients
- 72% said chemotherapy patients
- 67% said dialysis patients
- 59% said outpatient surgery centers
- 53% said dental
- 47% said vision
- 41% said regular outpatients (ENT, family practice, GI, internal medicine, nephrology, OBGYN)
About the Real Time Barometer
The Real Time Barometer is an observational study of the impact of the COVID-19 outbreak as reported by physicians with firsthand experience of treating COVID-19 patients. Each week, thousands of physicians provide insights on topics regarding the global health crisis. To date, more than 40,000 doctors in 31 countries, including the United States, Canada, United Kingdom, France, Brazil, Russia, China, Japan and Australia, have participated in the Barometer.
About Sermo
Sermo is the largest healthcare data collection company and social platform for physicians, reaching 1,3MM healthcare professionals across 150 countries. The platform enables doctors to anonymously talk real-world medicine, review treatment options via our proprietary Drug Ratings platform, collectively solve patient cases, and participate in medical market research. For more information, visit sermo.com.
Media Contact:
Angela Crawford
201-417-9157
Azito35@gmail.com