Collaboration among physicians forms the cornerstone of positive patient outcomes. In today’s increasingly complex medical landscape, a single physician cannot always have all the answers, particularly in rare, unsolved, or highly complex patient cases.
By leveraging peer-to-peer collaboration, physicians can tap into a vast pool of collective knowledge, reducing diagnostic errors, improving patient satisfaction, and enhancing the quality of care. However, there are a few concerns regarding privacy and confidentiality that must be addressed for the best possible outcomes.
Why physicians must collaborate on patient cases

The role of peer-to-peer consultation in complex cases
The medical field is continuously evolving, and with it, the complexity of patient cases. The compound annual growth rate (CAGR) of healthcare data is projected to reach 36% by 2025, significantly outpacing other sectors like manufacturing and financial services. Peer-to-peer consultations are essential, especially when dealing with mountains of data, rare diseases, diagnostic dilemmas, or multifaceted treatment plans.
Handling rare and unsolved patient cases
Research suggests that rare diseases often go misdiagnosed or undiagnosed for extended periods, primarily because an individual physician may not have encountered the condition before. For example, a physician in one specialty might collaborate with a geneticist or a neurologist on a complex case involving a rare neurological disorder. Peer-to-peer consultation can expedite the diagnostic process, saving time and, more importantly, improving patient outcomes.
Second opinions and reduced diagnostic errors
A second opinion can drastically reduce the likelihood of a misdiagnosis. A study published in the Journal of the American Medical Association found that diagnostic errors affect 1 in 15 adults annually in outpatient care settings. Peer consultations help mitigate this by bringing different perspectives and experiences into decision-making.
Improved patient outcomes through collaborative care
Studies have consistently shown that collaborative care models lead to better patient outcomes. The Journal of American Medical Association found that groups of 2 to 9 physicians had a diagnostic accuracy of 85.6%, compared to 62.5% for individual physicians.
Take mental health care, for example. Collaborative care models have proven to be an evidence-based method for improving patients across the board, with over 80 randomized controlled trials reporting that it makes mental health more accessible. A staggering 75% of patients on a collaborative model of care were able to get the behavioral care they need within six months compared to 25% of patients in a traditional, individual system.
By integrating multiple specialties and perspectives, physicians can create comprehensive care plans that address every aspect of a patient’s health and not just the plan a physician is accustomed to prescribing. Research highlights that collaborative care models are especially effective for chronic diseases like diabetes, depression, or hypertension and patients often experience better-controlled symptoms, lower hospital readmission rates, and higher overall satisfaction.
The risks of isolated decision-making in medicine

Diagnostic errors due to limited perspectives
Isolated decision-making, where a physician works without consulting peers, increases the risk of errors. A physician’s clinical knowledge is inherently limited to their personal experience and training. When multiple specialists collaborate, these limitations are reduced, allowing for a more accurate diagnosis and better treatment planning.
Increased risk of burnout and stress
Isolation in clinical decision-making is also linked to physician burnout. The burden of sole responsibility for complex patient cases can lead to stress and mental fatigue. Being able to talk candidly with peers reduces this strain by distributing responsibility and fostering a sense of support.
Delayed diagnosis and treatment
Each physician only has so much time and energy in a day. When physicians hesitate to seek external input, it can result in delays in diagnosis and treatment, negatively impacting patient outcomes. Peer collaboration ensures that different perspectives are brought in early, preventing treatment delays and delegating work to those best suited for the case.
The traditional methods of physician collaboration: risks and areas for improvement

Traditional case collaboration methods
Before digital platforms, physicians relied on in-person consultations, phone calls, or emails to collaborate on patient cases. While these methods have been widely used, they come with significant limitations and risks.
In-person consultations
In-person consultations, although valuable, are often time-consuming and not always feasible, especially when working with physicians in distant locations or in-demand specialties. Scheduling conflicts and geographic barriers can delay critical decision-making or limit access to care.
Email and text-based consultations
While convenient, email and text consultations pose significant security risks. Sensitive patient data shared via these methods can easily be intercepted, leading to data breaches and violations of patient privacy. Emails and texts can also be easily lost or overlooked, resulting in miscommunication or incomplete advice.
Limitations in data sharing and coordination
Traditional collaboration methods also lack the comprehensive data-sharing capabilities needed for effective decision-making. When physicians work with incomplete information, the quality of care suffers. Fragmented communication between healthcare providers often results in gaps in care, as seen in numerous studies examining care transitions.
How Sermo revolutionizes physician case collaboration
Sermo has transformed the way physicians collaborate by providing a secure, anonymous, and efficient platform for peer-to-peer consultation.
In this year alone, Sermo members have collaborated on over 25,000 patient cases together in real-time.
With over 1 million healthcare professionals (HCPs) in the community, Sermo offers unparalleled access to global medical expertise when you need it the most.
Benefits of using Sermo for physician case advice

Access to over 1 million physicians worldwide
The sheer size and depth of Sermo’s physician network across 96+ specialties offer unparalleled access to medical expertise. Whether you’re dealing with a rare disease or seeking advice on a complex surgical procedure, you can find physicians in almost every specialty who have dealt with similar cases and are eager to collaborate.
Honest drug reviews
Sermo has the world’s largest database of non-biased drug reviews in the world. Physicians just like you, who do not get paid for their review, are helping to improve treatment decisions through Sermo’s exclusive peer-to-peer Drug Ratings tool.
Specialty-specific discussion boards
Sermo’s discussion boards are tailored to specific medical specialties, allowing for more focused and relevant advice delivered straight to your feed. Physicians can engage with experts in their field, ensuring they receive the most specialized input available.
Secure environment for physician collaboration
Sermo validates every new member for security checks. We make sure each new member holds an active HCP license in good standing. We also offer anonymous patient case sharing and SSL-encryption to ensure that patient data remains protected under the strictest privacy and security regulations. Traditional methods of case collaboration, like email or phone, often fail to meet these standards, making Sermo a safe alternative for sharing sensitive patient information.
Real-time global peer network
With its global reach, Sermo enables physicians to connect with peers across different time zones, specialties, and countries. Physicians on Sermo report receiving responses to case consultations in a fraction of the time it would take using traditional methods. In urgent cases, this rapid turnaround can be life-saving.
Real-world impact: Case studies of successful collaborations on Sermo
Case study 1: a rare disease diagnosis solved
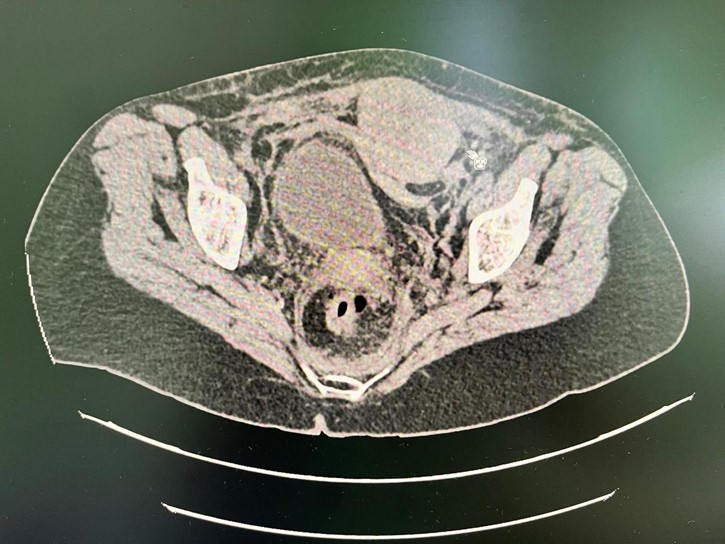
In one urgent case collaboration, a physician using Sermo presented a challenging case involving a female patient with severe abdominal symptoms. After consulting with our vetted community, the physician was able to confirm his diagnosis and treat the patient in time. The swift diagnosis enabled timely intervention, significantly improving the patient’s prognosis.
Case study 2: Multidisciplinary collaboration for cancer treatment
Another physician case involved a patient with an aggressive form of cancer. Through Sermo, an oncologist collaborated with surgeons and radiologists across several countries to aid her evaluation. The collective expertise allowed for a more personalized and effective approach, leading to better outcomes for the patient.
The future of physician collaboration: Embracing secure online platforms

Telemedicine and collaborative care
As telemedicine continues to grow, platforms like Sermo will play an increasingly important role in facilitating secure collaboration among healthcare providers. Physicians can consult with specialists from around the world without leaving their offices, bridging the gap between remote and in-person care.
Second opinions of AI analysis
As AI becomes more powerful and widespread in healthcare, online communities will provide a safe place to get second opinions about AI diagnosis and implementation recommendations. This ensures that AI assistance isn’t used in a vacuum where it can be dangerous.
Getting the most out of modern physician case collaboration
In an era where medical care is becoming more complex by the week, physician collaboration is more important than ever. Traditional methods of collaboration are fraught with inefficiencies and risks, especially when it comes to patient data security and timeliness.
Sermo provides a solution with a secure, real-time platform for global physician collaboration. It enables rapid peer-to-peer case advice and connects healthcare providers to a network of 1 million professionals, enhancing patient care through shared expertise.
Whether handling a rare disease, designing a multidisciplinary treatment plan, or seeking a second opinion, Sermo enables physicians to solve complex medical challenges collaboratively. This evolution in physician case collaboration moves medicine forward one discussion at a time.