By The Centers for Disease Control and Prevention (CDC)
While many people can benefit from PrEP, the majority of women who could benefit from PrEP aren’t currently receiving prescriptions for it. You can help change that by ensuring that all your patients consider PrEP as part of their comprehensive prevention plan.
Change is needed, and the numbers are convincing. Only one in 10 U.S. women who may benefit from PrEP were prescribed it in 2020. Yet, studies show that when taken as prescribed, PrEP reduces the risk of getting HIV from sex by 99% and from injection drug use by at least 74%. You can help combat these inequities by starting the conversation about PrEP with all your patients.
As a trusted source of health information, you can make a real difference in preventing HIV transmission. An advantage to PrEP is that it’s an HIV prevention method that a receptive partner can independently control. In fact, PrEP can help empower anyone to take control of protecting themselves from HIV.
CDC recommends providers talk about PrEP with all their sexually active adult and adolescent patients. CDC also recommends prescribing PrEP to women who are at risk for getting HIV. PrEP should be considered part of your patients’ comprehensive prevention plan that includes discussions about PrEP adherence, condom use, and other risk-reduction methods.
When it comes to PrEP medication, women have options. One option is Truvada® (or generic equivalent), which is currently the only oral PrEP medication approved for cisgender women. Descovy® is a second oral medication that is approved for use by transgender women. CDC now also recommends intramuscular cabotegravir (Apretude®) injections for anyone who might benefit from PrEP.
Empowering patients starts with a conversation, and this conversation starts with you. You can access free CDC patient resources on PrEP for women to help your patients determine if PrEP is right for them.
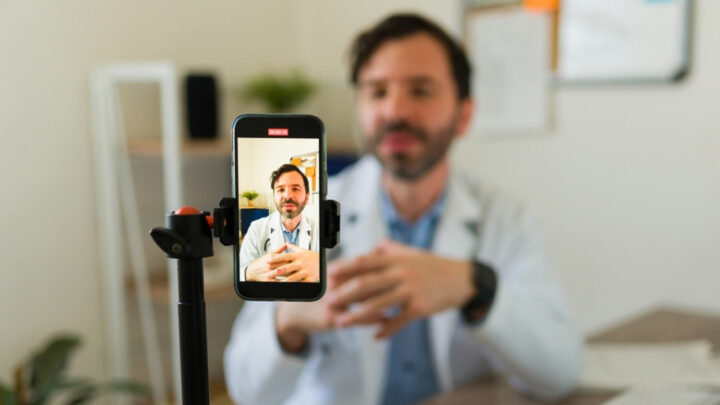
Our CDC clinical ambassadors offer their thoughts on PrEP:
When I talk about PrEP, I talk about it as being one component of HIV prevention. And when I have conversations with my patients around their general prevention care, we look at the whole picture. How many sexual contacts are they having, what kind of barrier method are they using, are they having conversations with their partners or contacts about their testing, and really making sure that they understand that PrEP is one piece of their general prevention care.
Ariel Watriss, MSN, NP-C
PrEP really has been a game-changer in many ways. PrEP is an incredibly exiting tool that we have in our HIV toolkit that we can offer to patients.
Oni Blackstock, MD, MHS
I think there’s work to be done about getting more people who would benefit from PrEP on treatment and addressing some of the barriers, but I think it has a lot of potential.
John Weiser, MD